Cancer Commun:贝伐珠单抗生物类似物LY01008对比贝伐珠单抗(Avastin)一线治疗中国不可切除、转移或复发的非鳞状非小细胞肺癌患者的疗效和安全性:一项多中心、随机、双盲III期试验
2021-07-01 yd2015 MedSci原创
中国晚期或复发非鳞状非小细胞肺癌(NSCLC)中,LY01008跟Avastin的疗效以及安全性相当。
肺癌是全球常见的恶性肿瘤。免疫时代到来之前,对于驱动基因阴性晚期非鳞状非小细胞肺癌(NSCLC)的治疗,抗血管治疗是重要的组成药物。贝伐珠单抗(Avastin)是常用的抗血管药物。LY0100是我国研发的贝伐珠单抗生物类似物。药理学和毒理学研究表明,LY01008与Avastin在临床前药效学、药代动力学和安全性方面是一致的。来自我国中国科学院肿瘤医院的石远凯教授开展了一项III期临床研究(NCT03533127),评估LY01008联合紫杉醇/卡铂对比Avastin联合紫杉醇/卡铂一线治疗中国晚期或复发性非鳞NSCLC的疗效和安全性,以验证两种药物的临床相似性。相关结果发表在Cancer Communications杂志上。
该研究是在我国67个研究中心开展的多中心、随机、双盲的III期临床研究。主要研究终点为客观缓解率(ORR),次要研究终点为疾病控制率(DCR)、疗效持续时间(DoR)、无进展生存期(PFS)、总生存期(OS和安全性。
649例患者随机分配至LY01008治疗组324例,Avastin组为325例。2019年9月25日进行主要研究终点分析,589例患者进行ORR评估分析,中位治疗周期数为5周期(范围1-6),中位治疗持续时间为3个月(范围:0-5.1)。LY01008组和Avastin组ORR分别为48.5%和53.0%。分层ORR比值为0.91 (90% CI 0.80-1.04,在预先规定的等效边界0.75-1.33内)。在大多数亚组中,包括65岁患者、男性患者、腺癌患者、不同EGFR突变状态(突变或野生型)患者、吸烟状态(是或否)、转移数量(3或3)患者的ORR率均在预先确定的同等范围内。

亚组分析

疗效评估
截至2020年5月15日, LY01008组的ORR为56.0%,Avastin组为58.8%。ORR比为0.95 (90% CI = 0.85-1.07)。LY01008组DCR为95.6%,Avastin组DCR为93.6%。DCR风险比为1.03 (90% CI =0.99-1.06)。LY01008组和Avastin组中位DoR分别为5.62个月(95% CI = 4.96-6.87)和5.72个月(95% CI = 4.86-7.06)个月(P = 0.508)。中位PFS为7.16个月(95%CI 6.87-8.28)和7.10个月 (95% CI = 6.74-8.21)(P=0.812)。中位OS为24.38个月(95%CI 23.85-未达到)和22.97个月(95%CI 20.37-未达到)(P=0.479)。1年OS率分别为79.4%和78.1%。
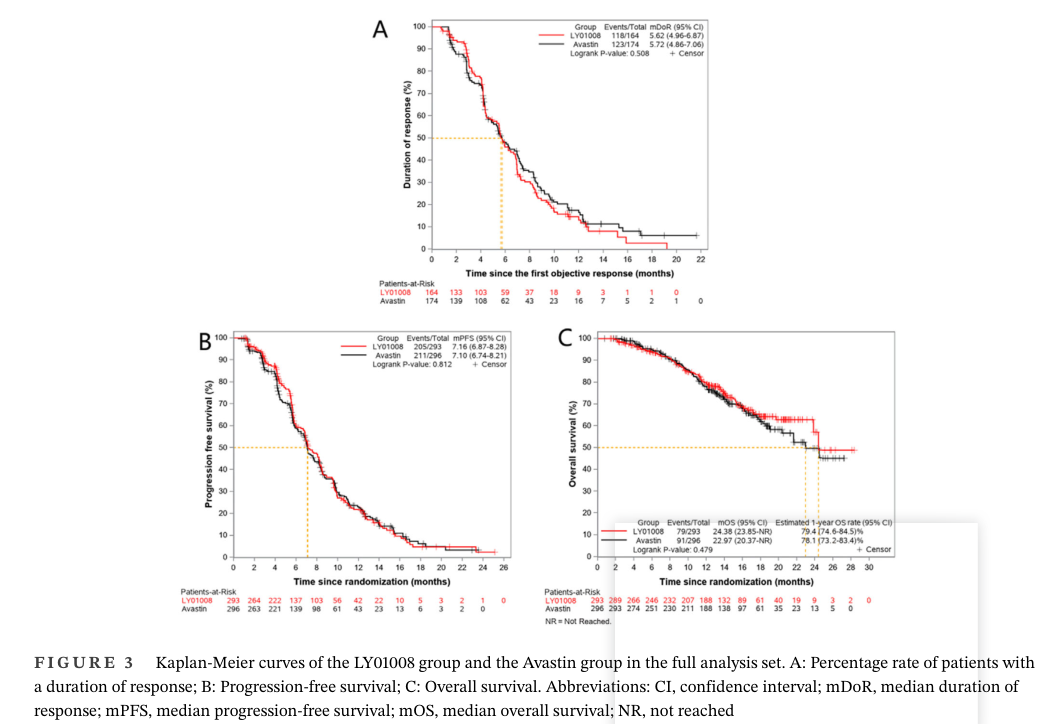
生存分析
两组的治疗相关不良事件(TEAEs)分别为99.1%和98.5%。大多数不良事件为1-2级。 LY01008组有78.3%和Avastin组有82.5%发生≥3级治疗相关不良事件。LY01008相关和Avastin相关TEAEs分别为73.7%和76.6%。3级LY01008相关和Avastin相关的TEAEs分别为37.8%和41.8%,其中LY01008组3级化疗药物相关的TEAEs有70.9%, Avastin组有77.2%。
综上,中国晚期或复发非鳞状非小细胞肺癌(NSCLC)中,LY01008跟Avastin的疗效以及安全性相当。因此LY01008联合紫杉醇/卡铂有希望成为一线治疗不可切除,转移性或复发非鳞状NSCLC患者的新选择。
原始出处:
Shi Y, Lei K, Jia Y, et al. Bevacizumab biosimilar LY01008 compared with bevacizumab (Avastin) as first-line treatment for Chinese patients with unresectable, metastatic, or recurrent non-squamous non-small-cell lung cancer: A multicenter, randomized, double-blinded, phase III trial. Cancer Commun (Lond). 2021 Jun 29. doi: 10.1002/cac2.12179. PMID: 34184418.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#VAST#
102
#贝伐珠#
50
#多中心#
54
#非小细胞#
52
#III#
47
#疗效和安全性#
43
#肺癌患者#
47
#II期试验#
74
#AST#
37
#COMMUN#
47