NEJM:结肠癌个体化辅助化疗新时代——究竟什么才是好的IDEA?
2018-03-29 Jenny 肿瘤资讯
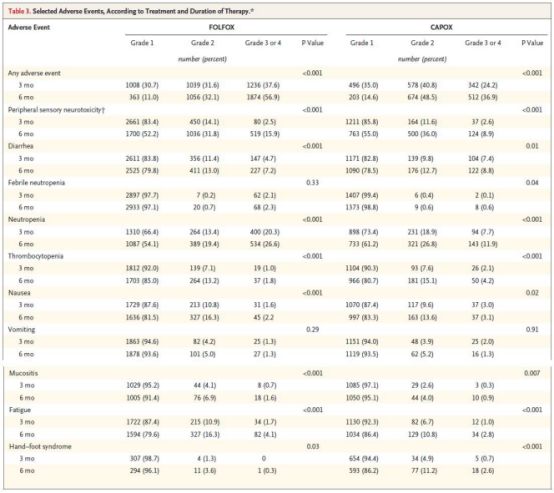
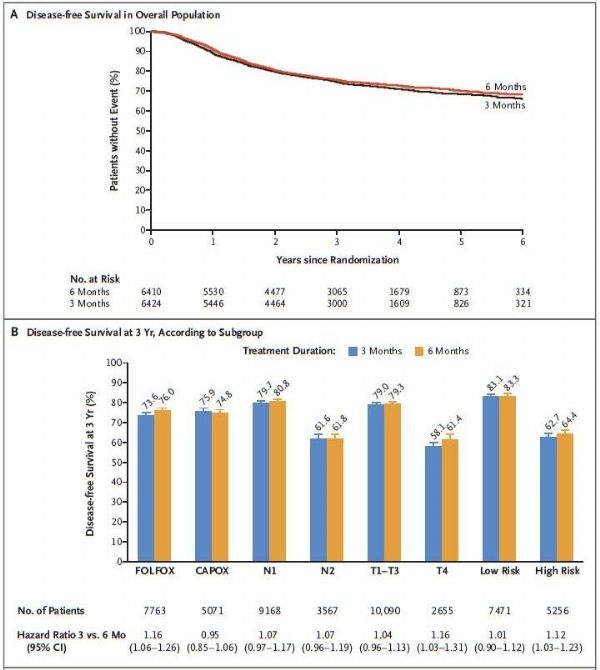
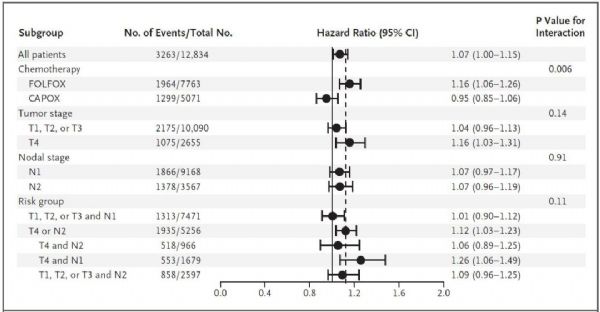
2017年无论是美国临床肿瘤学会年会(ASCO)还是欧洲肿瘤内科学会年会(ESMO),IDEA研究无疑是结直肠癌领域最热门话题之一。作为结肠癌史上样本量最大、时间跨度最长、多中心合作最多的前瞻性研究,IDEA也带来了前所未有的广泛争议。今天(2018年3月29日)《新英格兰医学杂志》(NEJM)在线发表了IDEA研究最终的全部结果,让我们先一睹为快!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习了谢谢分享!!
138
一起学习学习学习
120
学习了.谢谢
166
#个体化#
105
#新时代#
0
学习
109
很不错耶.学习了
94
学习了
92
学习了
85
内容丰富.知识面广
74