Sci Rep:日本科学家培养出能长毛发的皮肤
2016-04-03 孙学军 孙学军
皮肤是一个复杂的器官,对机体具有防水、缓冲、保护深层组织,排泄废物和体温调节等重要功能。日本学者开发出一种新的体内移植,成功建立了一个三维生物工程皮肤培养系统,这种皮肤拥有皮肤附属器官,如毛囊和皮脂腺。该方法利用诱导干细胞为基础的三维立体皮肤培养组织能在裸鼠移植存活,可以正确地宿主周围组织如表皮、竖毛肌和神经纤维融合,并不会产生肿瘤。这种生物工程立体皮肤组织还显示出毛发增生,产生包括毛囊干细胞的毛
皮肤是一个复杂的器官,对机体具有防水、缓冲、保护深层组织,排泄废物和体温调节等重要功能。日本学者开发出一种新的体内移植,成功建立了一个三维生物工程皮肤培养系统,这种皮肤拥有皮肤附属器官,如毛囊和皮脂腺。该方法利用诱导干细胞为基础的三维立体皮肤培养组织能在裸鼠移植存活,可以正确地宿主周围组织如表皮、竖毛肌和神经纤维融合,并不会产生肿瘤。这种生物工程立体皮肤组织还显示出毛发增生,产生包括毛囊干细胞的毛囊结构。这种皮肤组织在烧伤和整形学领域具有非常重要的应用前景。
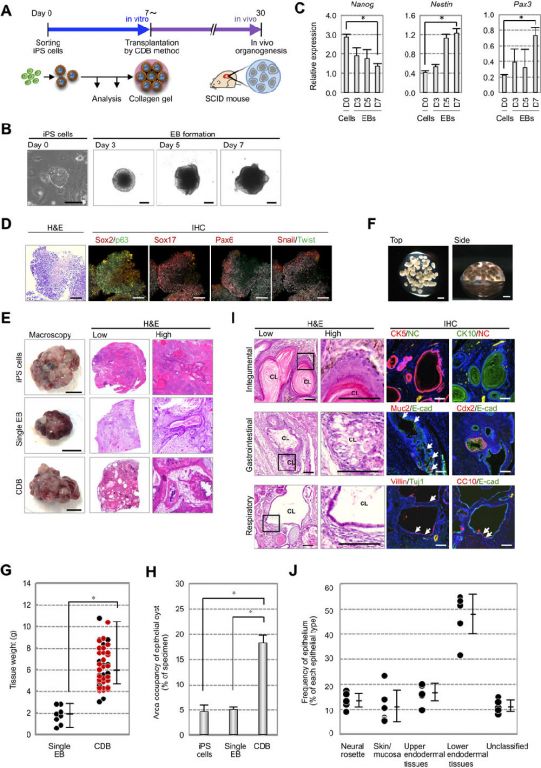
日本科学家用诱导干细胞成功培育出人工皮肤。神奇的是,这种小鼠牙龈组织诱导的干细胞为基础,制造的皮肤拥有完整的皮肤附属结构,例如毛发和皮脂腺。这一成功是皮肤再生医学领域的重要突破,将给烧伤和整形外科的发展提供了关键技术保障。将这种人工皮肤移植给裸鼠,这种动物缺乏免疫排斥能力,人工皮肤移植物与宿主融合理想,并能长出毛发。研究人员预测,将用5-10年把这种技术应用于临床。
研究小组希望可以利用烧伤患者自体组织培育出皮肤,这样就不需要考虑异体组织移植存在的免疫排斥问题。当然,如果这种技术成功,任何人希望对自身外表进行改造和修补,就会非常方便。整形外科一贯担心的皮瓣移植存在坏死的问题,也迎刃而解,因为可以不用采集自体皮肤,只需要用少量细胞就可以随意制造出有功能的皮肤组织。
这一技术也将为皮肤病和化妆品研究提供重要材料,过去这类研究都是用动物模型,以后可以用人工培养的人类皮肤,而且可以针对不同的皮肤类型如油性皮肤和干性皮肤等,选择性进行研究。
这一研究刚刚在《科学进展》杂志在线发表,该杂志是《科学》旗下(MedSci纠正:是自然出版社旗下)开放获取期刊,可以免费全文阅读。论文资深作者是Takashi Tsuji博士指出,过去人工皮肤研究上最大障碍是缺乏毛发腺体等必要的附属器官。导致人工皮肤缺乏必要的功能。最新技术成功地制造出更真实的皮肤组织,已经接近实现可以临床应用人工皮肤的梦想。

Tsuji博士来自神户发育生物学中心,最新研究是和东京和仙台等机构的同事合作进行的。首先从小鼠牙龈采集细胞,将这些细胞诱导成诱导干细胞iPS。诱导干细胞是干细胞领域的热门和流行研究技术。首先在2006年被报道,将成熟细胞进行化学改造,使它们时光倒流,返回到干细胞状态。诱导干细胞类似于胚胎,能不断进行分裂,
伦敦国王学院分子皮肤学教授John McGrath说,这项研究是该领域一直希望实现的目标,这是一个重大进步。对解决人类日益增长的皮肤功能疾病,这一研究给临床带来了曙光。虽然现在临床上已经开展人工皮肤移植,但是并没有实现皮肤功能的移植。因为这些皮肤缺乏毛发,也没有汗腺,缺乏皮肤的基本功能。
McGrath教授说,将会有许多实验室重复这一新发现,并将这种技术向临床应用转化。
原始出处:
Funao H, Nagai S, Sasaki A, Hoshikawa T, Tsuji T, Okada Y, Koyasu S, Toyama Y, Nakamura M, Aizawa M, Matsumoto M, Ishii K. A novel hydroxyapatite film coated with ionic silver via inositol hexaphosphate chelation prevents implant-associated infection. Sci Rep. 2016 Mar 17;6:23238. doi: 10.1038/srep23238.
PDF (1.3M)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#本科#
54
植发成为可能
170
植发成为可能
137
#日本#
91
期待临床验证
249
很有意思,这个很快应用临床吗
205
很有意思,这个很快应用临床吗
205
很有意思,这个很快应用临床吗
113
很有意思,这个很快应用临床吗
204
很有意思,这个很快应用临床吗
153