你计算的发病率,正确吗?
2017-07-23 大仙儿 医咖会
一、问题来了2014年,Li G等[1]在《Lancet Diabetes Endocrinol》杂志上发表的研究中报告了累计发病率(Cumulative Incidence)。累计发病率又称为累积发病率,是一个衡量疾病流行强度的指标。那么,累计发病率应该怎么计算呢?二、get新技能假设某研究者要探究糖耐量受损(IGT)人群中糖尿病的发病情况,筛选出了6例IGT的研究对象(为便于理解与计算,假定的
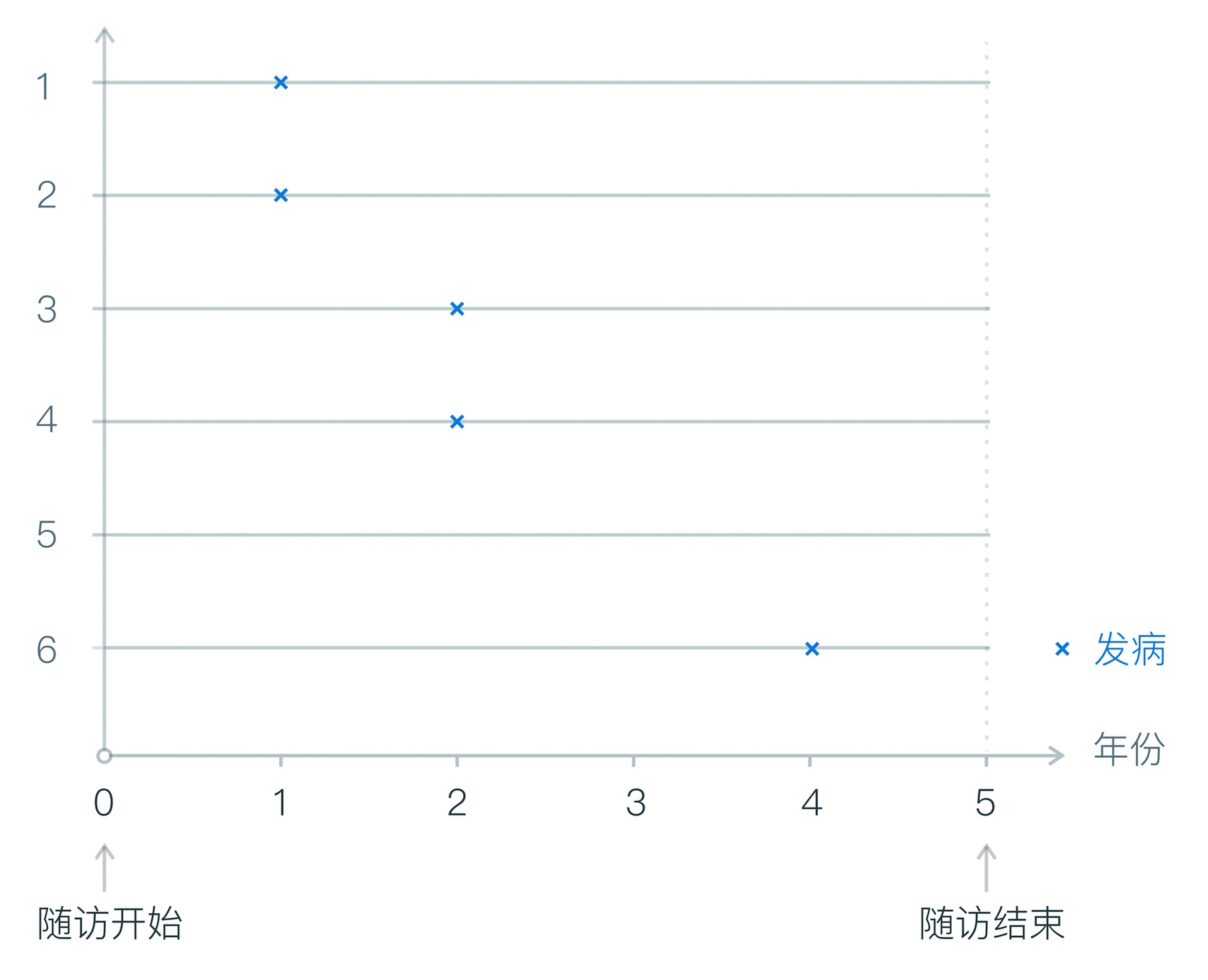
一、问题来了2014年,Li G等[1]在《Lancet Diabetes Endocrinol》杂志上发表的研究中报告了累计发病率(Cumulative Incidence)。累计发病率又称为累积发病率,是一个衡量疾病流行强度的指标。那么,累计发病率应该怎么计算呢?二、get新技能假设某研究者要探究糖耐量受损(IGT)人群中糖尿病的发病情况,筛选出了6例IGT的研究对象(为便于理解与计算,假定的人数较少,也未设定对照组),然后持续随访,观察糖尿病的发病情况(如随访示意图1所示)。 随访示意图1该研究有如下特点:①所有研究对象都是可能患糖尿病的IGT人群;②所有研究对象在观察期内保持稳定,都被观察了相同的时间。在有这样特点的研究中,累计发病率应该怎么计算呢?累计发病率 = 一定时间段内新发病例数 / 研究开始时的总人数 × 100% 该研究中,糖尿病的累计发病为:1年的累计发病率为2/6=33.3%2年的累计发病率为4/6=66.7%3年的累计发病率为4/6=66.7%4年的累计发病率为5/6=83.3%5年的累计发病率为5/6=83.3%可见,累计发病率随着随访
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发病率#
83
学习了.感谢!
100
学习了谢谢分享
107
非常专业的讲解
98
非常优质的讲解
108
专业!
101
这篇文章很有帮助
57
很有用的文章,非常感谢
53
谢谢分享,很不错。
53