European Urology:定量和定性分析液体活检对前列腺癌临床决策的指导作用
2021-01-12 MedSci原创 MedSci原创
最近的研究提供了对前列腺癌(PC)分子景观的见解,识别预后的生物标志物、可操作的靶点和耐药的生物标志物。难以获得合适的肿瘤材料进行分子检测是阻碍基因组图谱临床应用的原因之一。原发性前列腺肿瘤活组织检查
最近的研究提供了对前列腺癌(PC)分子景观的见解,识别预后的生物标志物、可操作的靶点和耐药的生物标志物。难以获得合适的肿瘤材料进行分子检测是阻碍基因组图谱临床应用的原因之一。原发性前列腺肿瘤活组织检查虽然是常规的,但在产量上往往不足,固定过程影响DNA质量。对标准治疗的雄激素受体(AR)靶向药物的二次耐药性通常涉及多克隆方式的基因组变化,这可能与后续治疗路线的选择有关。单个肿瘤活检,无论是原发性还是转移性病变,其捕获空间异质性的能力都是有限的,尤其是对于重复的纵向评估。事实上,原发性PC是最具空间异质性和克隆复杂的癌症类型之一。
液体活检的概念包括分析存在于体液中的肿瘤物质。这种物质可以以生物分子(如循环肿瘤DNA [ctDNA]、RNA、蛋白质和线粒体DNA)、循环肿瘤细胞(CTCs)或细胞外囊泡(EVs)的形式存在。液体活组织检查已成为一种极具吸引力的方法,以微创方式研究肿瘤分子景观,允许对整个肿瘤负荷进行实时快照。此外,基于液体活检的生物标志物可以作为临床试验的早期终点,以加快药物开发。
近日,发表European Urology的一篇新研究在回顾了目前基于血液的液体活检组件的知识,它们对PC临床决策的影响,加速精准医疗的机会,以及在临床实践中实施此类测试的挑战。
研究者对PubMed/MEDLINE数据库进行系统回顾,以确定2005年至2020年7月间发表的有关PC中CTCs、ctDNA和EVs的文献。选择涉及PC患者血液中CTCs、ctDNA和EVs的文章,并考虑其中引用的文献。
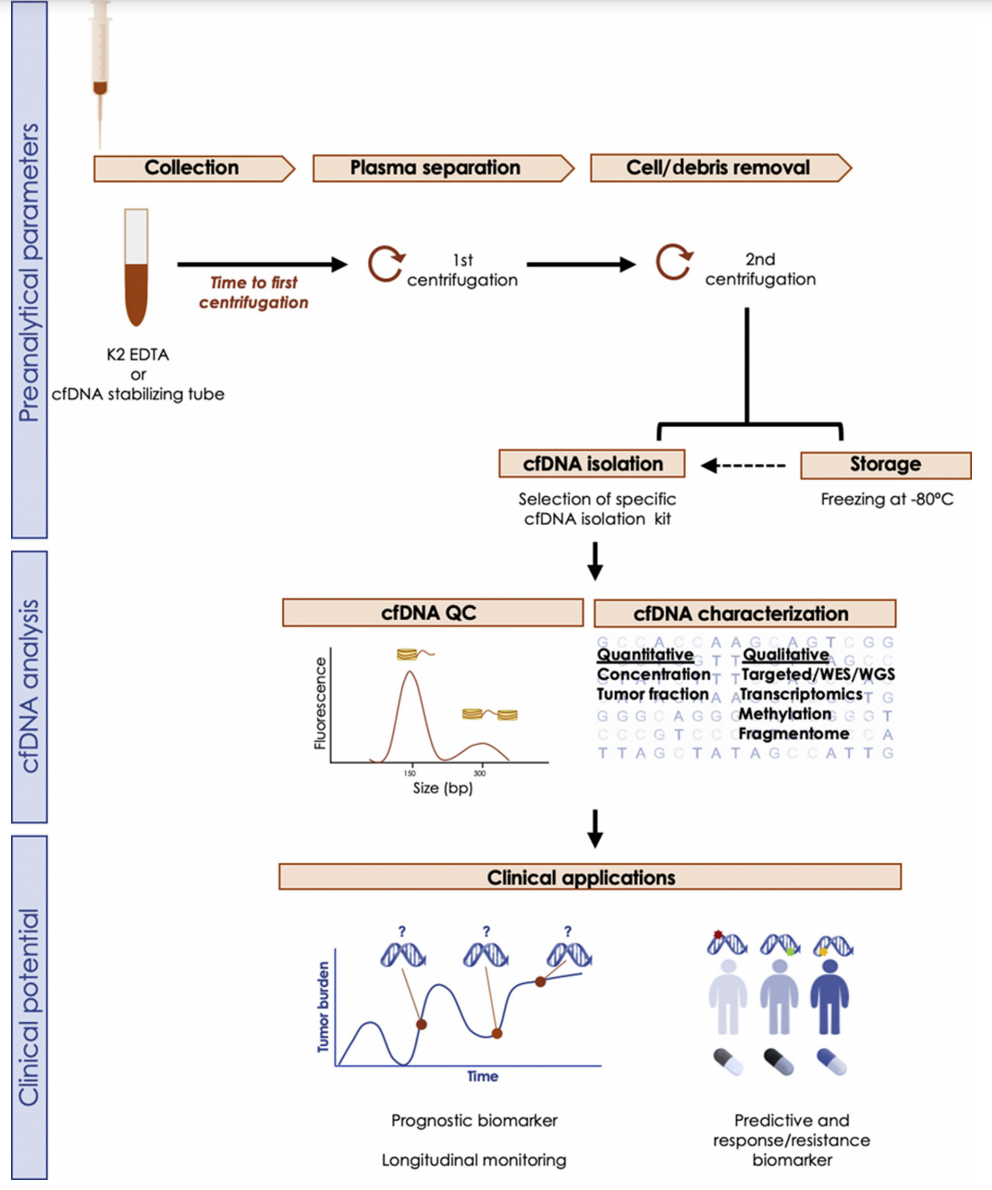
上图描述了血液的cfDNA研究的分析前、分析和分析后步骤的工作流程。静脉穿刺后,用含有抗凝剂(EDTA和柠檬酸盐优于肝素)的试管收集血液。从样品采集到处理的时间是至关重要的,因为cfDNA在几小时内就会降解。为了克服这个问题,可以使用含有不同DNA稳定剂的试管;这些管的使用在集中分析的大型多中心研究中特别相关,或者一般情况下,当样本在采集点没有处理时。建议采用两步离心法分离血浆成分,从血浆中提取cfDNA。如果不立即提取cfDNA,血浆可在80℃下保存较长时间,尽管反复冻融循环会增加非肿瘤DNA污染,从而损害cfDNA质量。在cfDNA分离后,在鉴定之前要进行质量控制(QC)测试,以评估cfDNA浓度和片段大小。
这篇综述指出,作者从四个方面分析了如何将液体活检技术应用于PC的临床治疗:定量预后和反应的生物标志物加速药物开发、局限性前列腺癌的临床应用、精确使用AR靶向制剂的液体活检和靶向治疗的预测生物标志物。
液体活检可以加速生物标志物的发展,以实现PC的精确护理。随着新的生物标志物驱动的治疗方法得到验证,液体活检也代表了一个机会,促进基因组检测在社区实践中的实施,转移性活检在社区实践中进行的比在学术中心更少。
CTC作为预后和反应性生物标志物的价值已经被清楚地证明,为加速药物开发和潜在地指导治疗决策提供了一个替代生物标志物。然而,成本和获取技术,以及在CTC定义和分离平台方面的研究之间的异质性,使CTC分析转换为常规临床试验变得复杂。初步研究表明,ctDNA动力学在临床实践中可能也是一种有用的预后和反应性生物标志物,尽管还需要进一步的临床试验资质。由于CTCs和ctDNA均产生平行的肿瘤负荷,因此在局部疾病中的适用性可能具有挑战性,尽管随着超灵敏检测方法的发展,液体活检可能有潜力帮助监测根治性治疗后的患者,或补充基于组织的生物标记物以改善患者分层。在临床环境中使用EVs有希望,可以补充CTC和ctDNA分析,但在隔离方法的标准化和下游应用方面面临挑战。
此外,对液体活检分析的新特征的研究,如片段组学(基于ctDNA片段大小)、起源组织分析和甲基化分析,可能对早期肿瘤阶段提供信息。重要的是,由于液体活检可以揭示多种分析物更广泛的突变情况,将这些复杂的多维数据集成到复合生物标记物中是当前的需求,也是该领域的一个活跃研究领域。
总之,在过去的十年里,PC的液体活组织检查领域取得了指数级的进步,发展了预后和预测生物标志物,并为监测肿瘤进化的微创手段带来了希望。液体活检可以指导治疗决策,加速PC精准医学的发展。然而,需要解决的问题包括测定方法的灵敏度和特异性的标准化,不同测定方法的前瞻性临床鉴定,以及成本和可及性,以支持其在常规临床实践中的实施。
参考文献:Irene Casanova-Salas , et al. Quantitative and Qualitative Analysis of Blood-based Liquid 4 Biopsies to Inform Clinical Decision-making in Prostate Cancer. European Urology January 06, 2021, DOI:https://doi.org/10.1016/j.eururo.2020.12.037
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床决策#
93
#PE#
86
#活检#
70
#决策#
75
赞
167
前列腺癌相关研究,学习了,谢谢梅斯
100
学习了
98
#学习#学习了
96