Br J Cancer:系统性评估和荟萃分析揭示浸润性T细胞标志物在宫颈癌发生中的作用
2020-12-11 xiaozeng MedSci原创
子宫颈癌作为最常见的妇科肿瘤之一,在全球范围内具有较高的发病率和死亡率,在2018年有超过569,000例病例和311,000例死亡病例。尽管目前在高收入人群中的筛查已大大降低了子宫颈癌的发病率,且随
子宫颈癌作为最常见的妇科肿瘤之一,在全球范围内具有较高的发病率和死亡率,在2018年有超过569,000例病例和311,000例死亡病例。尽管目前在高收入人群中的筛查已大大降低了子宫颈癌的发病率,且随着疫苗接种计划的进行将进一步降低该病的发病率,然而,疫苗接种和常规筛查的差异也后导致发病率的巨大差异。
感染致癌性人乳头瘤病毒(HPV)是宫颈癌的必要原因之一。超过90%的HPV感染会在两年内自发清除。宿主的适应性免疫应答有助于确定子宫颈HPV感染是否持续存在并发展为癌前和癌症,而T细胞浸润的系统表征则有助于了解子宫颈癌发生发展的关键步骤。
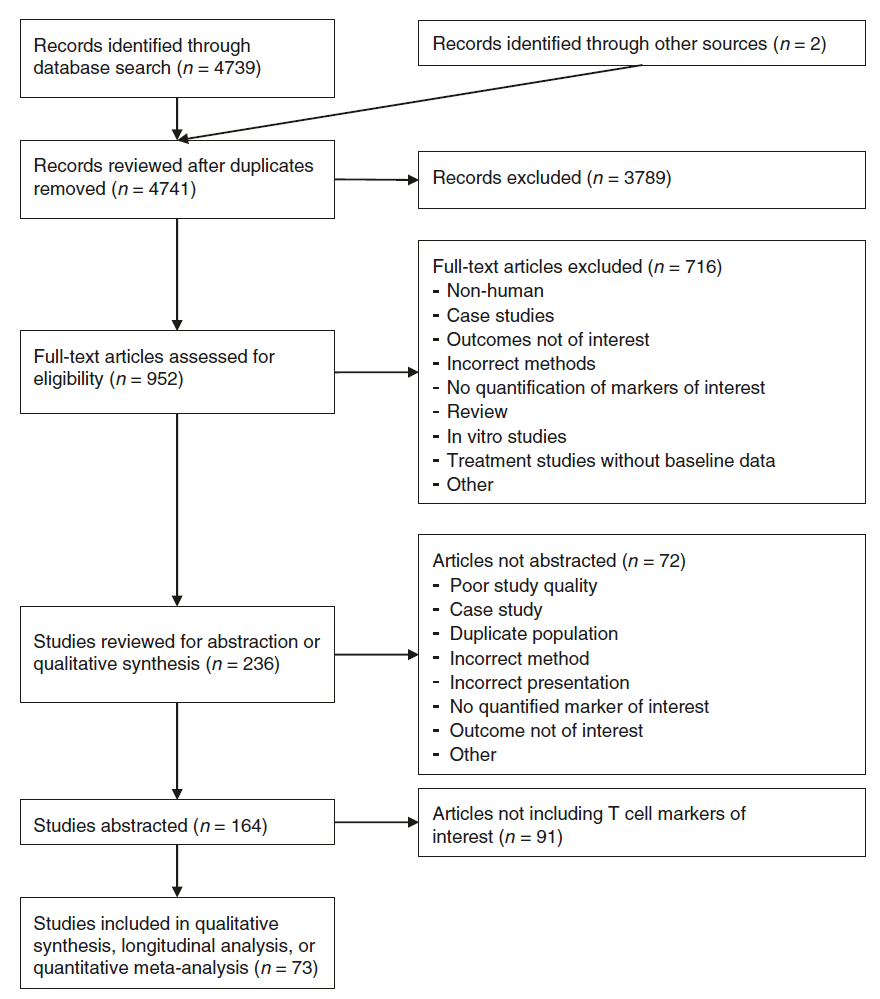
该研究对正常宫颈、低度病变、高度病变和浸润性癌中的浸润性T细胞进行系统性评估和荟萃分析,包括上皮、基质和总组织以及相关的标记物分析:CD3、CD4、CD8、FoxP3、CD25和CD4:CD8比例。另一项定性评估总结了浸润性T细胞与宫颈疾病的持续性、消退、发生发展以及预后相关性的纵向数据。
流程图
研究人员发现,相比于正常上皮,宫颈病变中的CD3+,CD4+和CD8+细胞更少,而癌症中这些细胞更多。在持续性和癌前病变中,FoxP3和CD25+调节性T细胞的浸润率很高,纵向数据显示,较低的调节性T细胞水平可改善患者的预后。
该研究结果显示,成功的免疫逃逸可以减少HPV感染和癌前上皮细胞中的T细胞浸润反应,而浸润性癌症具有高度的免疫原性,且随着宫颈疾病的发展,调节性T细胞的浸润也会增加。
浸润性T细胞在宫颈癌发生中的概念模型
因此,了解这些因素具有潜在的预后价值,其或可为开发新的治疗方法和临床指南提供一定的指导。
原始出处:
Litwin, T.R., Irvin, S.R., Chornock, R.L. et al. Infiltrating T-cell markers in cervical carcinogenesis: a systematic review and meta-analysis. Br J Cancer (01 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
56
#荟萃#
69
学习
118
#荟萃分析#
58
#标志物#
57
学习
153
学习
131
#宫颈#
54
学习
119
高收入人群中的筛查已大大降低了子宫颈癌的发病率,疫苗接种计划的进行将进一步降低该病的发病率,疫苗接种和常规筛查的差异也后导致发病率的巨大差异。女性的疾病希望更多广大医学从业者给予重视,
133