Nature:重磅!单个CAR-T细胞让癌症患者5年内保持无癌状态
2018-06-06 佚名 细胞
在一项新的研究中,来自美国宾夕法尼亚大学艾布拉姆森癌症中心的研究人员报道一名慢性淋巴细胞白血病(CLL)患者在2013年接受嵌合抗原受体(chimeric antigen receptor, CAR)T细胞(CAR-T细胞)治疗后因单个CAR-T细胞及其增殖时产生的细胞而发生病情缓解,从那以后在5年内保持无癌症状态,并且这些CAR-T细胞仍然存在于他的免疫系统中。他们还证实这种治疗反应与CAR编码
在一项新的研究中,来自美国宾夕法尼亚大学艾布拉姆森癌症中心的研究人员报道一名慢性淋巴细胞白血病(CLL)患者在2013年接受嵌合抗原受体(chimeric antigen receptor, CAR)T细胞(CAR-T细胞)治疗后因单个CAR-T细胞及其增殖时产生的细胞而发生病情缓解,从那以后在5年内保持无癌症状态,并且这些CAR-T细胞仍然存在于他的免疫系统中。他们还证实这种治疗反应与CAR编码基因插入到这名患者的T细胞DNA中的位置相关联,这可能是有助于提高这种治疗反应率的一种关键因素。相关研究结果于2018年5月30日在线发表在Nature期刊上,论文标题为“Disruption of TET2 promotes the therapeutic efficacy of CD19-targeted T cells”。论文通信作者为宾夕法尼亚大学艾布拉姆森癌症中心的J. Joseph Melenhorst博士和Carl June博士。

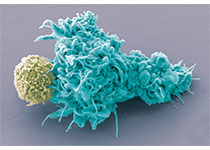
图片来自Nature, doi:doi:10.1038/s41586-018-0178-z。
作为一种癌症,CLL起源自产生骨髓中的某些白细胞(即淋巴细胞)的细胞。这些癌细胞首先在骨髓中出现,随后迁移到血液和淋巴结中。这些癌细胞增值得太快,将骨髓中的其他细胞挤出。它们并没有正常地成熟,因而不能够像它们应当的那样抵抗感染。美国癌症协会估计2018年将有约21000例新的CLL病例,并且大约有4500例死于这种疾病。这些患者中的许多人将接受骨髓移植,但是另一种可能的治疗方法就是CAR-T细胞疗法,它涉及收集患者自身的T细胞,对它们进行重编程而使得它们能够识别和杀死癌症,然后将它们灌注回到患者体内。这种方法已被美国食品药物管理局(FDA)批准用于治疗某些急性淋巴细胞白血病(ALL)患者以及一些非霍奇金淋巴瘤患者,但是当前尚未批准用于治疗CLL。
为了控制细胞因子释放综合征(CRS),患者通常接受三次连续灌注,灌注剂量分别为10%、30%和60%。CRS是一种与CAR-T细胞疗法相关的常见毒副作用,包括不同程度的流感样症状,伴有发热、恶心和肌肉疼痛,并且可能需要重症监护室(ICU)级别的护理。这项研究报道的这名患者接受了前两次剂量分别为10%和30%的灌注,但是他起初并没有产生治疗反应。Melenhorst说,“直到第50天时,这名患者才经历CRS,这表明这些CAR-T细胞具有活性并可能发挥抗肿瘤作用。”
成像结果显示这名患者的肿瘤在变小,因此医生们决定最后为他进行剂量为60%的灌注。这名患者进入缓解状态,并保持缓解状态5年了而且还在继续保持这种状态。June说,“这是我们一直期待的结果,不过我们知道,无论如何,我们都能够从每名患者那里学到很多。我们将这种结果从床边带到实验台以便尽可能多地理解发生了什么和为何会如此。”
论文第一作者、宾夕法尼亚大学艾布拉姆森癌症中心的Joseph A. Fraietta博士说,“我们发现的第一件事是我们能够将这名患者的CAR-T细胞谱系追溯到单个原始细胞。这是一个非常了不起的发现,这基本上告诉我们CAR-T细胞完成它们的任务所需的最低剂量是一个细胞。”
Fraietta 说,“这名患者的CAR-T细胞经基因改造后寻找白血病细胞表面上的一种被称作CD19的蛋白。在这种策略中,编码识别CD19蛋白的CAR的基因被一种经过基因修饰的病毒随机地插入到这名患者的DNA中。就这个特定的病例而言,这些研究人员发现CAR序列插入到一个被称作TET2的基因中,其中在正常情形下,TET2基因调节血细胞的形成,并限制这些细胞的生长。一旦TET2基因被破坏,单个CAR-T细胞大量增殖并消灭这名患者所患的白血病。通常抵抗感染的杀伤T细胞不能单独地战胜癌症,这是因为它们衰老了,过了辉煌期,而且经常寡不敌众。然而,更年轻的CAR-T细胞让一切变得与众不同,这是因为它们能够大量增殖,形成为一个效应T细胞群体。在这种情形下,它们有机会发挥作用,这是因为TET2受到抑制,不再影响促进这种治疗反应产生的表观遗传通路。”
2012年,宾夕法尼亚大学和诺华公司开始进行全球合作,推动进一步的研究、开发和商业化被称作Kymriah(之前称作CTL019的)的CAR-T细胞疗法和其他的CAR T细胞疗法用于治疗癌症。2017年8月,FDA批准Kymriah用于治疗25岁以下患有难治性的或复发性的B细胞前体ALL的患者。2018年5月,这种批准得到扩展,可用于治疗复发性的或难治性的弥漫大B细胞淋巴瘤(DLBCL)---最常见的非霍奇金淋巴瘤形式---成人患者以及高度B细胞淋巴瘤(high grade B-cell lymphoma)和起源自滤泡性淋巴瘤的DLBCL。
原始出处:
Joseph A. Fraietta, Christopher L. Nobles, Morgan A. Sammons et al. Disruption of TET2 promotes the therapeutic efficacy of CD19-targeted T cells. Nature, Published online:30 May 2018, doi:10.1038/s41586-018-0178-z
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#无癌状态#
62
#Nat#
52
#CAR-#
45
#癌症患者#
47
#重磅#
48
学习学习谢谢分享
88
学习了.长知识
70