JAMA Cardiol:他汀类药物治疗与冠脉粥样硬化斑块进展的关系
2021-10-12 Nebula MedSci原创
他汀类药物的使用与冠状动脉粥样硬化向高密度钙转化的发生率更高有关
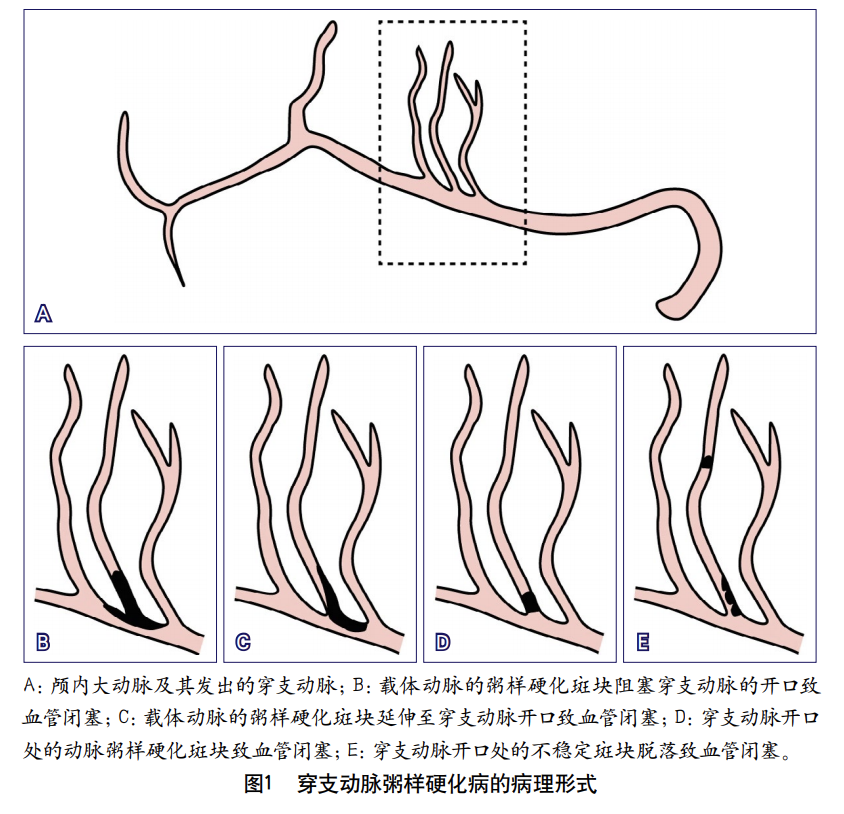
冠状动脉粥样硬化斑块负担与未来主要心血管事件的风险增加有关。动脉粥样硬化斑块的密度是区分斑块钙化和非钙化形态的基础。
这是一项在7个国家开展的队列研究,旨在评估粥样硬化斑块密度的变化对动脉粥样硬化疾病进展的指示作用,招募了间隔2年或2年以上连续接受冠脉CT血管造影检查的患者。主要终点是单个冠脉斑块的斑块组成进展。根据斑块衰减程度,在体素水平上定义了6种斑块组成类型:低衰减 (-30~75 HU)、纤维脂质成分 (76-130 HU)、纤维性的 (131-350 HU)、低密度钙化 (351-700 HU)、高低度钙化 (701-1000 HU) 和1K (>1000 HU)。根据他汀类药物使用和基线斑块体积之间的相互作用评估这6种斑块类型的进展率,并根据危险因素和检查间隔时间进行调整。
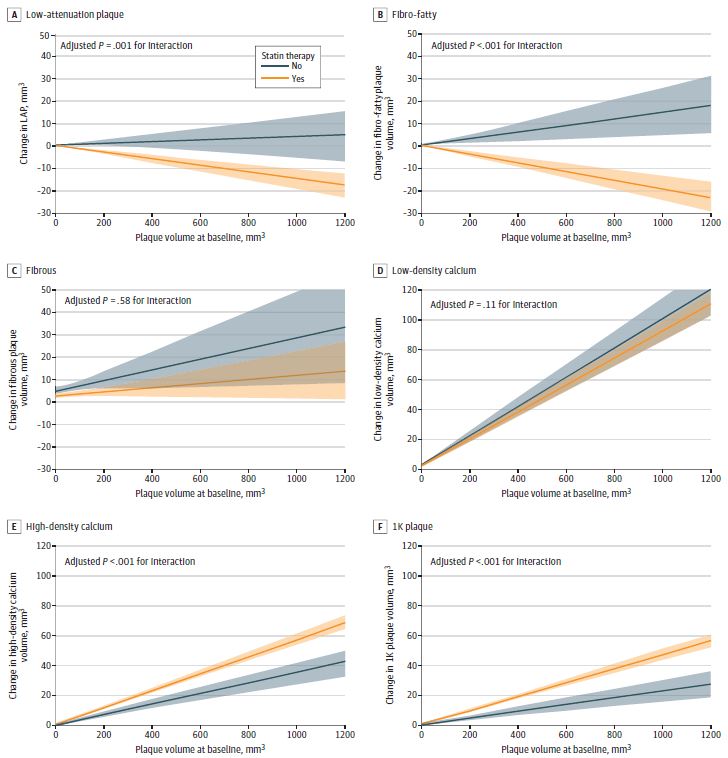
根据基线斑块体积和他汀类药物使用分组的斑块变化
2013年至2016年期间,招募了857位患者(平均62.1岁,63.0%的男性;63.9%的接受他汀类药物治疗),共2458处冠脉斑块被纳入分析。在所有6种斑块类型中,未经治疗的斑块的体积都随时间的推移有所增大。他汀类药物治疗与低减斑块(β -0.02; p=0.001)和纤维脂肪斑块(β -0.03; p<0.001)的体积减少相关;但他汀类药物治疗还与高密度钙化斑块(β 0.02; p<0.01)和1K斑块(β 0.02; p<0.001)进展更大相关。
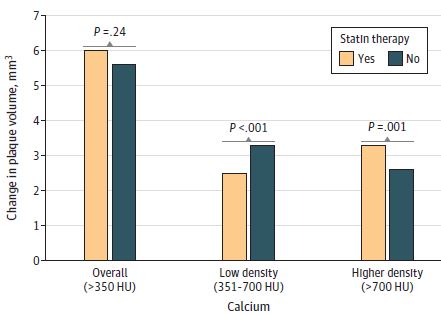
他汀类药物与钙化密度的相关性
当分析仅限于基线时无低衰减斑块或纤维脂肪斑块的病变时,他汀类药物治疗与钙化斑块总体积的变化无关(β -0.03; p=0.24),但与病变斑块向更致密的钙化转变有关。基线斑块体积和钙密度之间的相互作用分析显示,冠脉钙密度越大,斑块进展越少。
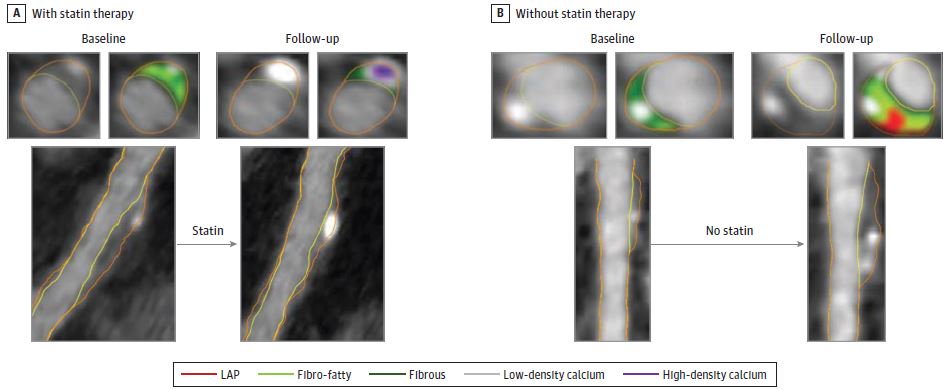
有无使用他汀类药物的冠脉粥样硬化进展
该研究结果表明,他汀类药物的使用与冠状动脉粥样硬化向高密度钙转化的发生率更高有关。随着斑块密度的增加,斑块整体进展的速度变慢。该研究结果支持,钙密度增加可降低动脉粥样硬化风险的观点。
原始出处:
van Rosendael AR, van den Hoogen IJ, Gianni U, et al. Association of Statin Treatment With Progression of Coronary Atherosclerotic Plaque Composition. JAMA Cardiol. Published online August 18, 2021. doi:10.1001/jamacardio.2021.3055
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiol#
61
#他汀类药#
71
#粥样硬化#
61
#斑块#
62
学习了,他汀的另一作用
89
学习了
96
学习学习
91
学习了
89
太坑人呢台历足球比赛呢
87
学习
44