JCEM:进食氨基酸同样能产生肠促胰素效应
2015-01-19 angletears 译 MedSci原创
肠促胰素效应,是指同等量的葡萄糖,口服比静脉注射更能促进移动啊素分泌,这与肠道分泌的两种肠促胰岛素,GIP和GLP-1有关。据研究,口服葡萄糖后,70%-80%的胰岛素分泌与肠促胰素效应有关。但是,这种肠促胰素效应不仅仅只存在于碳水化合物,很可能与其他宏观营养素有关。之前,来自瑞典的Ola Lindgren和他的团队,已经证明,这种肠促胰素效应,在进食脂质时同样存在。最近,他们的研究进一步证明,进
肠促胰素效应,是指同等量的葡萄糖,口服比静脉注射更能促进移动啊素分泌,这与肠道分泌的两种肠促胰岛素,GIP和GLP-1有关。据研究,口服葡萄糖后,70%-80%的胰岛素分泌与肠促胰素效应有关。但是,这种肠促胰素效应不仅仅只存在于碳水化合物,很可能与其他宏观营养素有关。之前,来自瑞典的Ola Lindgren和他的团队,已经证明,这种肠促胰素效应,在进食脂质时同样存在。最近,他们的研究进一步证明,进食氨基酸同样产生肠促胰素效应。
研究者选取12位男性非糖尿病志愿者,平均年龄在22.5±1.4岁,平均BMI22.4±1.4 kg/m2,,分别给予相同浓度的氨基酸口服或静脉注射。
试验中,测量餐后120min的胰岛素、C肽、胰高血糖素、GLP-1、GIP的曲线下面积(AUC),及胰岛素分泌率和胰岛素清除率
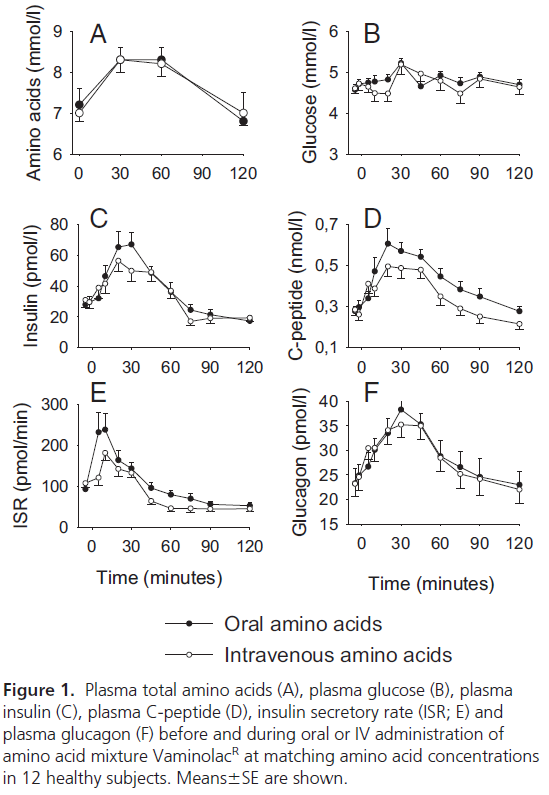
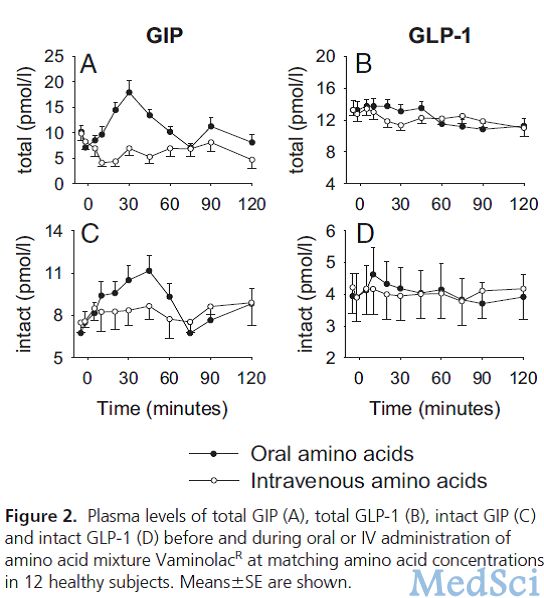
结果,胰岛素、C肽、胰高血糖素水平在口服和静脉注射氨基酸时,均升高了。但是,口服氨基酸时,胰岛素的分泌率比静脉注射的高25%。然而,胰高血糖素的反应在口服和静脉注射两种情况下,并无差别。
他们得出结论,给予同等水平的氨基酸,口服比静脉注射,可促进更多的胰岛素分泌,这与餐后GIP的水平迅速升高有关,这提示,口服氨基酸后引发的肠促胰岛素效应,很可能是由GIP介导的。
本文是MedSci原创编译整理,欢迎转载!转载请注明来源并附原文链接。谢谢!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
45
#肠促胰素#
63
#氨基酸#
51
#JCEM#
39
#进食#
56