BMJ:美国不同心脏病亚型死亡负担变化研究(1999-2018)
2020-08-19 MedSci原创 MedSci原创
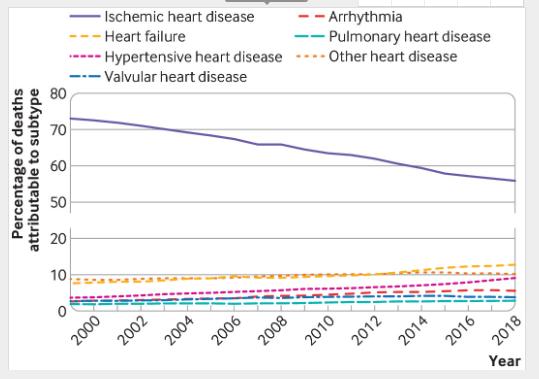
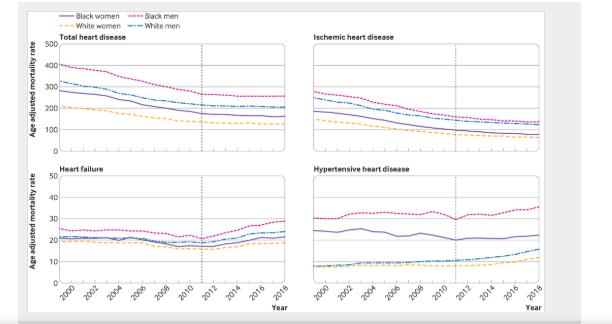
自2011年以来,缺血性心脏病患者的死亡率趋于缓解,但心力衰竭和高血压性心脏病的潜在风险不断增加。以高危人群为重点,早期和有针对性的心脏病危险因素的预防和控制是必要的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习
83
#BMJ#
59
#死亡负担#
80
了解
122