常见消化道瘘的影像学表现--膀胱肠瘘
2015-02-03 首都医科大学附属北京朝阳医院 蒋涛 中国医学论坛报
膀胱肠瘘多发生于膀胱及邻近结肠、小肠、直肠、阑尾及乙状结肠,结肠憩室、炎症、结肠或膀胱肿瘤浸润或放疗后并发症是形成瘘的主要原因。 膀胱造影和钡剂灌肠检查有意义的阳性发现为钡剂进入膀胱或膀胱造影剂进入肠道,并且直接显示瘘管,但此种检查的阳性率不高。 卡瓦纳(KavanaghD)等认为,CT平扫发现膀胱内积气或口服肠道造影剂进入膀胱;强化CT检查发现造影剂进入瘘管或肠道既可确诊本病,同
膀胱肠瘘多发生于膀胱及邻近结肠、小肠、直肠、阑尾及乙状结肠,结肠憩室、炎症、结肠或膀胱肿瘤浸润或放疗后并发症是形成瘘的主要原因。
膀胱造影和钡剂灌肠检查有意义的阳性发现为钡剂进入膀胱或膀胱造影剂进入肠道,并且直接显示瘘管,但此种检查的阳性率不高。
卡瓦纳(KavanaghD)等认为,CT平扫发现膀胱内积气或口服肠道造影剂进入膀胱;强化CT检查发现造影剂进入瘘管或肠道既可确诊本病,同时还可以提供膀胱内外的局部病变情况。
国内学者发现,膀胱内积气、局部膀胱壁增厚、膀胱外肿块是膀胱肠瘘最常见的影像表现。

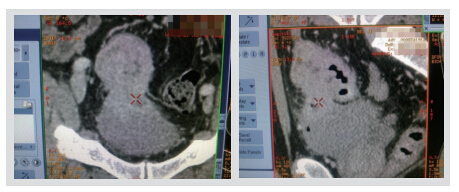
图1 患者男性,44岁,乙状结肠癌侵犯膀胱致乙状结肠-膀胱瘘,膀胱内可见气体影

图2 患者女性,55岁,子宫恶性肿瘤术后放疗后。膀胱壁明显增厚,膀胱-阴道-乙状结肠瘘
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







非常好的文章,学习
187
?学习了
136
?学习了
169
#消化道#
60
#肠瘘#
67
#肠瘘#
71