JAHA:乳头肌异常运动员ECG中T波倒置
2021-01-27 MedSci原创 MedSci原创
PMs肥大和心尖移位可能是运动员无法解释的侧向TWI的基础。PMs异常相关的侧向TWI为独特的临床症状,其特征是患者预后良好。
心脏乳头肌(PMs)异常可能与ECG复极异常有关。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估无临床确诊心脏病的运动员侧向T波倒置(TWI)与PMs特征之间的关系。
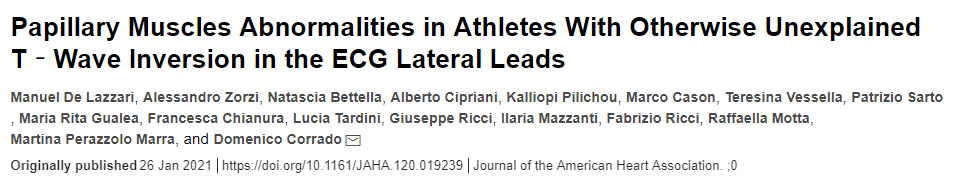
研究人员纳入了53名具有侧向TWI的运动员(中位年龄为20岁;男性为87%),他们在临床和心脏磁共振评估中也没有心脏病的证据。心电图正常的健康运动员作为对照组。研究人员评估了PMs的大小,例如直径、面积、体积、质量以及PMs与左心室质量之间的比值,以及PMs心尖移位的患病率。
与对照组相比,TWI运动员表现为PMs肥大,且PMs直径、面积、体积和质量显著增加。TWI运动员的PM与左心室质量之比为4.4%,而对照运动员为3.0%(P<0.001)。PMs/左心室质量比>3.5%用于区分TWI运动员和对照者的敏感性为85%,特异性为76%。在25名(47%)患有TWI的运动员中发现了PM的心尖移位,而9名(17%)对照组中发现了PMs心尖移位(P=0.001)。在多变量分析中,PMs/左心室质量比和心尖移位仍然是TWI的独立预测因子。尽管继续坚持运动,但TWI和PMs异常的运动员的临床结局仍然较为平稳。
由此可见,PMs肥大和心尖移位可能是运动员无法解释的侧向TWI的基础。PMs异常相关的侧向TWI为独特的临床症状,其特征是患者预后良好。
原始出处:
Manuel De Lazzari.et al.Papillary Muscles Abnormalities in Athletes With Otherwise Unexplained T‐Wave Inversion in the ECG Lateral Leads.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019239
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#T波倒置#
60
#AHA#
58
#ECG#
63
#运动员#
71
标题有误吧
100