Gut:胃肠化生的严重程度预测胃癌的发生:一项前瞻性队列研究(GCEP)
2021-05-13 yd2015 MedSci原创
胃肠化生(IM)是促进早期胃癌发生的危险因素,建议采用风险分层方法,并建议高危患者(OLGIM III-IV)在2年内接受内镜监测,中危患者(OLGIM II)在5年内接受内镜监测。
胃癌是常见的恶性肿瘤。常常因发现时已经处于晚期导致死亡居高不下。只有日本和韩国因为政府资助的内镜筛查项目,胃癌的死亡率极低,说明内镜筛查对于发现早期胃癌的重要性。胃癌的发生遵循可视化的癌前病变过程,从炎症、萎缩、肠化生(IM)、异常增生和癌变。胃肠化生的手术环节(OLGIM)常被用来评估胃肠化生的严重程度。
来自新加坡的研究团队发表了一项研究数据,评估在胃肠生化(IM)患者中早期胃癌(EGN)的发生率和利用OLGIM评估IM患者的严重程度。这是一项前瞻性、纵向和多中心研究,纳入新加坡胃癌流行病学、分子遗传计划项目2004年1月到2010年12月接受胃镜检查并标准化胃粘膜取样筛选的患者,并在第3年和第5年进行定期监测胃镜检查。参与者还与国家疾病登记办公室的早期胃肿瘤(EGN)漏诊匹配。

研究共纳入2980名患者,1321(n=44.3%)例患者发现IM。1541例患者为男性(51.7%); 47.8%有幽门螺杆菌感染病史; 22.2%患者既往或目前吸烟,14.2%患者有胃癌家族史。
在随访期间,共21例被诊断为EGN,包括13例高级别异常增生,和8 例IA/IB 期胃腺癌。多因素分析发现老年患者 (校正HR 1.08; 95% CI 1.02 to 1.16; p=0.02), 胃蛋白酶原阳性 (校正HR 4.23; 95% CI 1.34 to 13.37; p=0.01),萎缩性胃炎(校正HR 2.69; 95% CI 1.03 to 7.06; p=0.04)和IM(校正HR 5.36;95% CI 1.51至19.0;p<0.01)是EGN的重要危险因素。
经年龄调整后伴有或不伴有IM的EGN发生率为133.9/100和12.5/100 000人年。OLGIM III-IV期患者的风险最大(校正HR 20.7;95% CI 5.04至85.6;p<0.01)。一半以上的EGN(n=4/7)是由OLGIM III-IV患者在2年内(范围:12.7-44.8个月)发展来的。OLGIM III-IV期患者从基线的胃镜检查到发现早期胃癌具有较短的时间间隔(中位 22.7个月; 范围12.7–44.8个月),而OLGIM stage II患者为(中位 50.7个月; 范围 28.5–73.3个月),两者有显著统计学差异(p=0.01)。
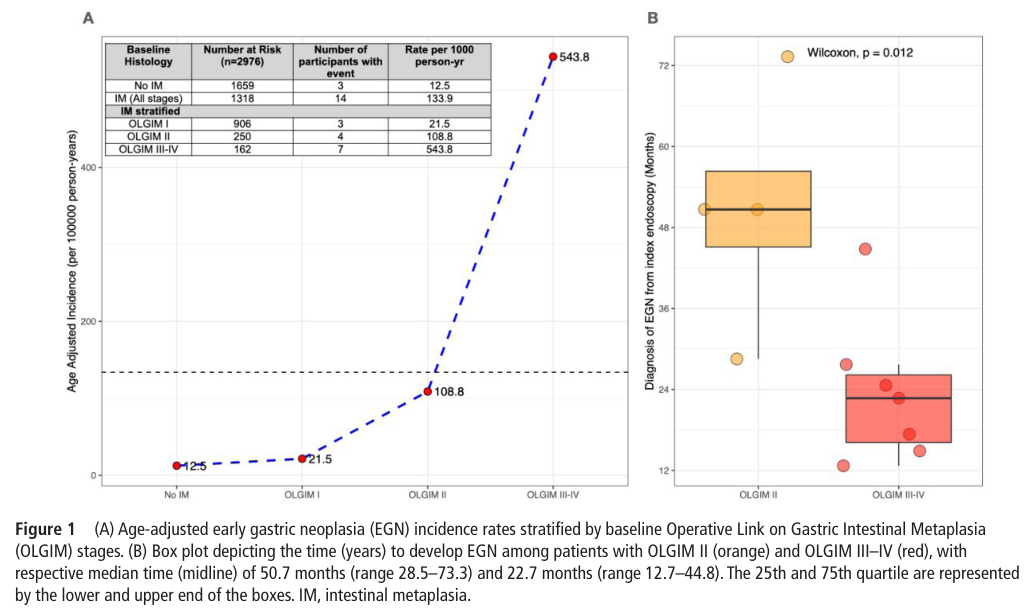
年龄调整EGN的发病率
研究者进一步筛查OLGIM高风险患者的血液标志物,主要关注TFF3, MIF 和 胃蛋白酶原 II/I比例。研究表明只有TFF3 能够鉴别HP阴性的OLGIM III–IV 和OLGIM 0–II 患者 (AUROC 0.749; 95% CI 0.628 to 0.870; p<0.01)。
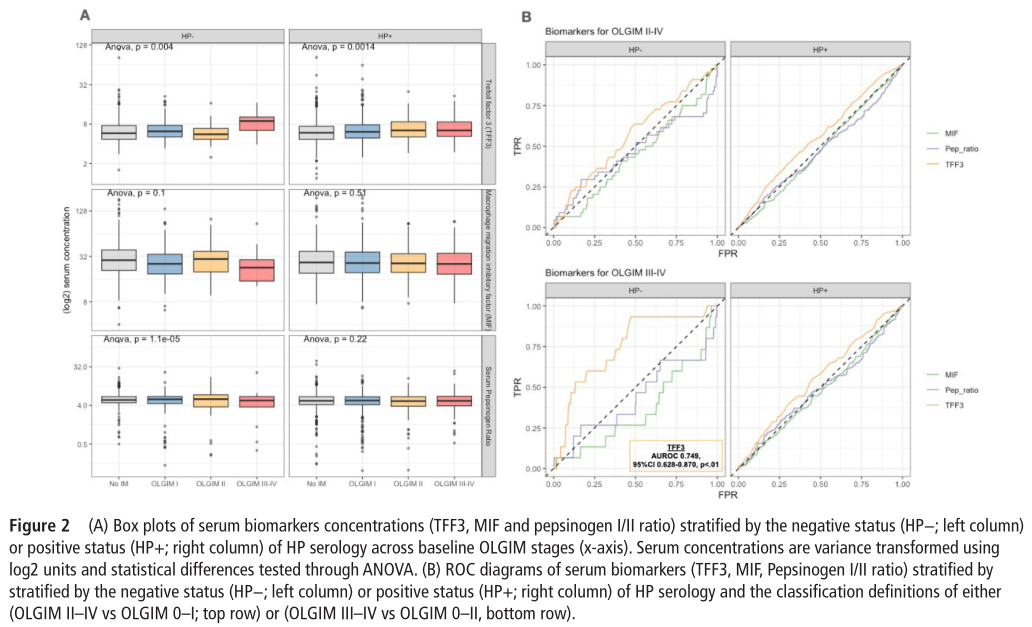
OLGIM高风险患者的血液标志物
接着研究将IM患者根据OLGIM分为四个等级,(i)逆转, (ii) 低风险, (iii) 中等风险,(iv) 高风险。随着OLGIM等级越高,IM逆转的比例越低。OLGIM III–IV 患者没有发现有逆转的。相反,只有一小部分基线OLGIM I的患者随后出现OLGIM II型(10%)和OLGIM III-IV型(3%)。血清胃蛋白酶原指数是OLGIM I转化为OLGIM II–IV的一个显著预测因子。血清胃蛋白酶原指数阳性的OLGIM I期患者,进展到更高阶段的可能性高出两倍(OR 5.81; 95% CI 2.26 - 14.9; P=0.01)。
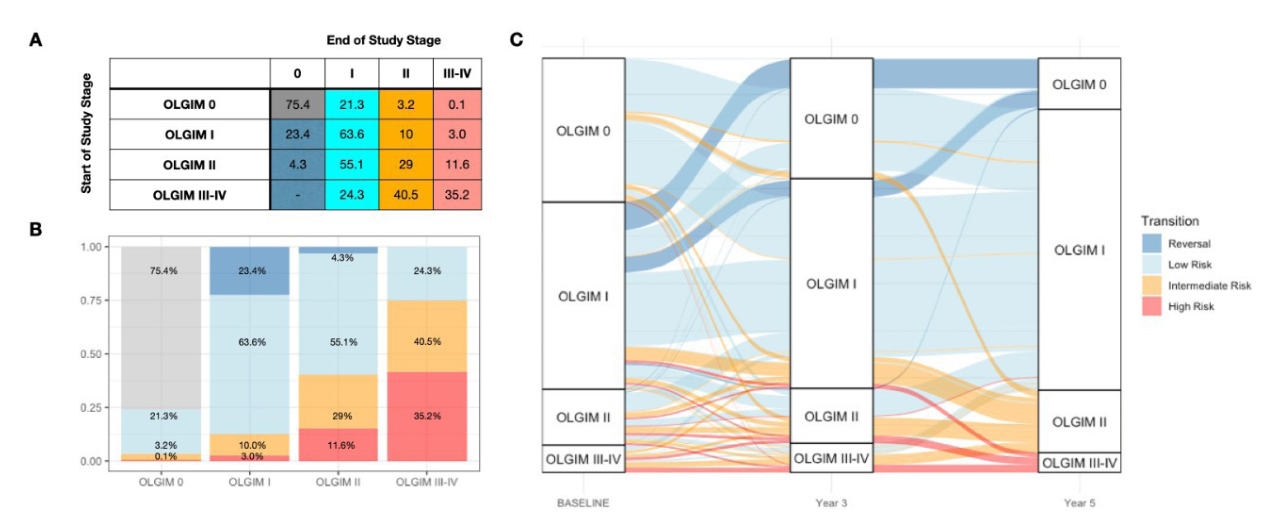
IM的转化
综上,IM是促进早期胃癌发生的危险因素,建议采用风险分层方法,并建议高危患者(OLGIM III-IV)在2年内接受内镜监测,中危患者(OLGIM II)在5年内接受内镜监测。
原始出处:
Lee JWJ, Zhu F, Srivastava S, et al. Severity of gastric intestinal metaplasia predicts the risk of gastric cancer: a prospective multicenter cohort study (GCEP). Gut. 2021 May 11; gutjnl-2021-324057. doi: 10.1136/gutjnl-2021-324057. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前瞻性队列研究#
84
#前瞻性队列#
107
#前瞻性#
53
#肠化生#
70
可以有
102