Eur J Cancer:术后辅助立体定向放疗可改善边缘切除的肝癌患者的生存预后
2022-03-21 xiaozeng MedSci原创
术后辅助立体定向放疗可显著改善边缘切除的肝细胞癌患者的无病生存率和总生存率
肝细胞癌(HCC)是全球第七常见的恶性肿瘤,其疾病相关死亡率居高不下。手术切除仍是早期肝癌的最重要的治愈性方案。但很多病人会复发,大大限制了长期生存率。可惜的是,目前尚无推荐的辅助治疗。
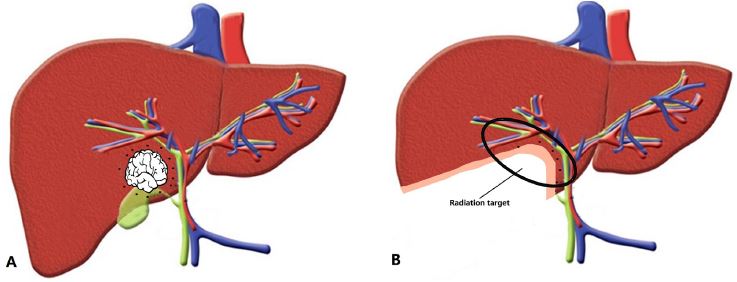
肝癌边缘切除示意图
肝癌的肝切除术多采用边缘切除,局部复发率高,特别是有微血管侵犯(MVI)的患者。立体定向放射治疗 (SBRT) 对肿瘤的控制和肿瘤血栓形成有明显疗效。本研究旨在探讨SBRT作为MVI阳性肝癌辅助治疗的疗效。
这是一项在上海东方医院肝胆外科开展的单中心、随机对照试验,纳入了MVI阳性的接受边缘切除的肝癌患者,随机分成了两组,接受手术+术后辅助SBRT或仅进行手术(SA)治疗。主要终点是无病生存率(DFS)和总生存率(OS);次要终点是不良反应。
两组的DFS
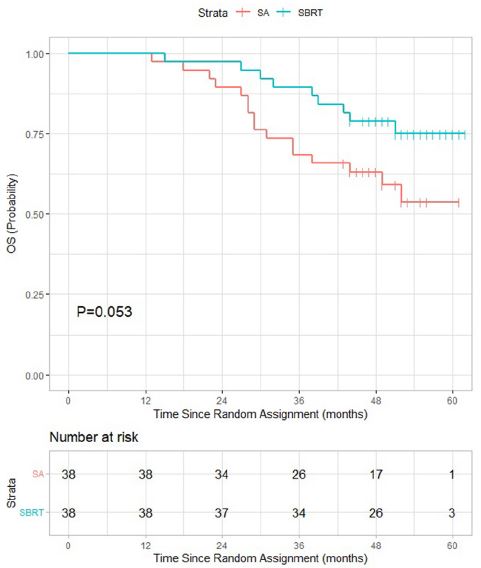
共招募了76位患者,每组各38位。中位随访了55个月后,共有44位患者复发,25位患者死于肝癌复发。SBRT组和SA组的一年、三年和五年无病生存率分别是92.1% vs 76.3%、65.8% vs 36.8%和56.1% vs 26.3%(p=0.005)。SBRT组和SA组的一年、三年和五年总生存率分别是100% vs 100%、89.5% vs 68.4%和75.0% vs 53.7%(p=0.053)。
两组的OS
单组SBRT总剂量为35 Gy,生物有效剂量 (BED) 为59.5 Gy。放疗相关不良事件的总发生率为31.6%(12/38),无3级及以上不良事件发生。
该研究表明,对于采用边缘切除的微血管侵犯的肝癌患者,术后辅助立体定向放疗可有效预防局部复发,提高无病生存率,且安全性好。
原始出处:
Shi Changying,Li Yong,Geng Li et al. Adjuvant stereotactic body radiotherapy after marginal resection for hepatocellular carcinoma with microvascular invasion: A randomised controlled trial.[J] .Eur J Cancer, 2022, 166: 176-184. https://doi.org/10.1016/j.ejca.2022.02.012
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#定向#
85
#立体定向#
84
#生存预后#
87
#肝癌患者#
107
#立体定向放疗#
108