Crit Care:感染性休克患者不同种糖皮质激素治疗有差异吗?
2017-03-29 xing.T MedSci原创
由此可见,没有明确的证据表明任何一个皮质激素药物或治疗方案可能会比其他治疗更有效在降低死亡率、减少胃肠道出血或感染性休克二重感染方面。氢化可的松静脉注射或输液可能比安慰剂和甲基强的松龙更容易导致休克逆转。
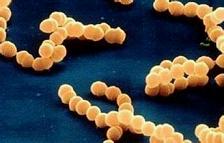
多种糖皮质激素和治疗方案已被用于感染性休克的辅助治疗,不同的药物及其给药模式之间在细胞和组织水平存在定性和定量的差异。近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,研究人员旨在明确不同糖皮质激素药物和它们的治疗方案在使用皮质类固醇激素的成年感染性休克患者结局上的任何差异。
研究人员对最近进行的Cochrane回顾的数据进行了网络荟萃分析。包含了儿童的研究,并且被设计来评估肺炎和急性呼吸窘迫综合征患者呼吸功能的研究,以及交叉研究,均被排除在外。研究人员为每一个结局生成了网络图,并且所有分析使用频率统计方法进行分析,假定为随机效应模型。
研究人员纳入了22个研究的完整数据以及1个研究的部分数据。网络荟萃分析没有提供明确的证据表明任何干预或治疗方案是优于任何其他治疗的,考虑到所有全部结局时。只有在一个方面即休克逆转上才有强有力的证据表明存在不同的差异。氢化可的松静脉注射和输液可能比甲基强的松龙静脉注射和安慰剂更容易诱导休克逆转。
由此可见,没有明确的证据表明任何一个皮质激素药物或治疗方案可能会比其他治疗更有效在降低死亡率、减少胃肠道出血或感染性休克二重感染方面。氢化可的松静脉注射或输液可能比安慰剂和甲基强的松龙更容易导致休克逆转。
原始出处:
Ben Gibbison, et al. Corticosteroids in septic shock: a systematic review and network meta-analysis.Critical Care.2017.http://ccforum.biomedcentral.com/articles/10.1186/s13054-017-1659-4
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#感染性#
54
#糖皮质#
37
#激素治疗#
48
#皮质激素#
41
文章很好,值得分享
73
学习了谢谢分享
65
很好的学习资料,谢谢!
81
很好的学习资料,谢谢了。
71
感谢分享一下!
62
学习了
0