盘点:脑瘤2016重要研究进展
2016-09-17 MedSci MedSci原创
脑癌是指生长在颅腔的新生物,又称颅内肿瘤、脑瘤,可起源于脑、脑膜、神经、血管及脑附件,或由身体的其他组织或脏器转移侵入颅内而形成,大都可产生头痛、颅内高压及局灶性症状。近年来,颅内肿瘤发病率呈上升趋势,颅内肿瘤约占全身肿瘤的5%,占儿童肿瘤的70%。恶性胶质瘤,源自神经上皮的肿瘤统称为胶质瘤(胶质细胞瘤),占颅脑肿瘤的40-50%,是最常见的颅内恶性肿瘤。在英国,每年有1.6万多人经诊断患
脑癌是指生长在颅腔的新生物,又称颅内肿瘤、脑瘤,可起源于脑、脑膜、神经、血管及脑附件,或由身体的其他组织或脏器转移侵入颅内而形成,大都可产生头痛、颅内高压及局灶性症状。近年来,颅内肿瘤发病率呈上升趋势,颅内肿瘤约占全身肿瘤的5%,占儿童肿瘤的70%。恶性胶质瘤,源自神经上皮的肿瘤统称为胶质瘤(胶质细胞瘤),占颅脑肿瘤的40-50%,是最常见的颅内恶性肿瘤。在英国,每年有1.6万多人经诊断患上脑瘤。不到20%的脑癌患者能够存活5年以上,相比之下,对乳腺癌患者而言,这一数字是87%,而对睾丸癌患者而言,这一数字是98%。这里小M整理了2016年以来关于脑瘤的重要研究进展与大家分享。
【1】 靶向致命脑瘤的癌症干细胞群体有望解决治疗抵抗和复发难题
近日,来自美国西北大学的研究人员通过研究找到了治疗多形性成胶质细胞瘤及神经胶质瘤干细胞的潜在靶点。多形性成胶质细胞瘤目前仍然是最致命的恶性脑瘤,而神经胶质瘤干细胞会促进治疗抵抗和肿瘤复发。
在这项最新研究中,研究人员发现MAPK作用激酶(MNK)是治疗多形性成胶质细胞瘤中神经胶质瘤干细胞群体的潜在靶点。研究分析表明相比于其他疾病亚型来说,间叶细胞样多形性成胶质细胞瘤的两个MNK基因(MKNK1和MKNK2)均发生表达上调。
研究人员利用病人来源细胞建立的细胞系进行研究发现使用肿瘤治疗药物LY2801653(merestinib)对MNK进行抑制能够进一步抑制真核翻译起始因子4E(eIF4E)的磷酸化水平,eIF4E是MNK诱导癌细胞进行mRNA翻译的一个重要执行因子,同时也是癌细胞转化的一个标记物。
更为重要的是,研究人员通过极限稀释分析方法发现merestinib能够抑制神经胶质瘤干细胞形成的神经球的生长,这表明肿瘤治疗药物merestinib可以作用于神经胶质瘤干细胞,有望解决这种致命脑瘤的治疗抵抗和复发难题。
研究人员通过颅骨内异种移植小鼠模型评估了merestinib在体内条件下的治疗效果,结果观察到接受药物治疗的小鼠其整体生存率得到了提高。(文章详见——Mol Cancer Res:靶向致命脑瘤的癌症干细胞群体有望解决治疗抵抗和复发难题)

【2】 高等教育会增加患脑瘤风险
通过大量的研究表明,高程度教育会增加患脑瘤的风险,研究显示,在大学学习至少3年的人比那些没有进入高等学府教育的人患神经胶质瘤的机率大。
研究人员的发现是基于对超过430万瑞典人的研究分析得出的数据,在观察期间有110万人死亡,超过48,000人是移民,这些人中有5735名男性和7101名女性患上了脑瘤。
相比受教育程度不超过义务教育时期(9年)的男性,接受至少三年大学教育的男性有19%的可能会产生一种神经胶质瘤,这是一种在神经胶质细胞中产生的癌变肿瘤,神经胶质细胞会包绕并保护大脑中神经元的发育。相比没有接受高等教育的女性,接受至少三年大学教育的女性患神经胶质瘤的风险会高达23%,并且有16%的患脑膜瘤的风险,这是一种大多是在脑膜层组织中产生的良性脑瘤。脑膜层组织包绕并保护大脑和脊髓。
大量的可支配收入可增加14%男性罹患神经胶质瘤的风险,但对脑膜瘤和听神经瘤没有影响,听神经瘤是一种良性脑瘤,该肿瘤产生在用于听力和平衡的神经中。任何类型的可支配收入都不会增加女性患脑瘤的风险。
职业似乎也影响男性和女性患脑瘤的风险。与从事体力劳动的男性相比,半体力半脑力和非体力工作者罹患神经胶质瘤的风险达到20%,罹患听神经瘤的风险达到50%。
相比从事体力劳动工作的女性,从事专业管理工作的工作者患神经胶质瘤的风险高出26%。相比已婚或未婚的同居男性,单身男性患神经胶质瘤的风险较低,但是单身男性患脑膜瘤的风险较高。然而在女性中没有明显的这种关联。(文章详见——JECH:高等教育会增加患脑瘤风险)
【3】 脑瘤治疗重大突破!液态阿司匹林杀死脑癌细胞的效率比化疗提高10倍!
脑瘤 2016---从生物学到治疗国际研究会议上,一项潜在里程碑性的科学突破对未来的脑瘤治疗产生极其深远的影响。依据这项突破性的研究,含有液态阿司匹林的饮料可能能够延长上千名脑癌患者的寿命。
研究人员发现这种简单的药物能够穿过血脑屏障---它阻止化疗药物攻击脑瘤。他们宣布了早期的测试结果:相比于现存的任何一种化疗药物,液态阿司匹林杀死脑癌细胞的效率提高了10倍。
他们利用来自患上一种常见的被称作胶质母细胞瘤(glioblastoma)的侵袭性脑瘤的成年人和儿童的脑癌细胞测试了这种如今被称作IP1867B的液态阿司匹林溶液。他们发现IP1867B在疗效上比任何当前使用的其他药物组合强10倍。
这是因为阿司匹林本身就具有杀死癌细胞的能力。但是,如果他们将抗癌药物加入到这种溶液中---他们已经在开始测试---的话,他们期待这种治疗的威力得到显著改善。这种溶液中的三种组分已被批准在人体内使用,这意味着相比于其他的新药,它的临床试验应当会更快开展。(文章详见——脑瘤治疗重大突破!液态阿司匹林杀死脑癌细胞的效率比化疗提高10倍!)
【4】 脊髓灰质炎病毒可治疗脑瘤
近日杜克健康中心的Preston Robert Tisch脑瘤研究中心的一项研究显示,改良型脊髓灰质炎病毒治疗复发的脑胶质瘤患者可以延长患者的生存期。该研究结果发表在近日举行的美国临床肿瘤学会年会(ASCO)上。
经改良的脊髓灰质炎病毒将不良作用降低到最低,可以汇集到癌细胞表面含量比较丰富的某种受体。改良的病毒进入肿瘤细胞并成功感染肿瘤细胞,从而激活免疫反应。
Desjardins和同事报告了首批15例患者的研究结果。在首批治疗中,使用的病毒剂量不断增加,以测试所能达到的最大效果。为了更好地进行对比,研究者纳入了124例对照病例,这124例患者未进行脊髓灰质炎病毒治疗,并且年龄、性别、身体状况、疾病进展情况等均与接受病毒治疗的患者相当。
截止今年1月,接受病毒治疗的患者的中位生存期为12.6个月,而未进行病毒治疗的患者的中位生存期为10.5个月。试验进行到第24个月时,接受病毒治疗的患者中有20%仍存活,而该数据在未进行病毒治疗的患者中只有13.7%。(文章详见——ASCO 2016:脊髓灰质炎病毒可治疗脑瘤?)
【5】 ASCO 2016:放疗后进行化疗或可有效改善罕见脑瘤患者的生存率
2016年美国临床肿瘤学会年会上的一项研究报告中,来自欧洲癌症研究与治疗协作组等机构的研究人员通过研究表示,放疗后进行化学疗法或可有效减缓一种罕见脑瘤的生长,从而使得第5年生存的癌症患者的比例从44%增加至56%。
研究者进行的这项III期临床试验中,他们比较了那些并不太会对化疗产生反应的癌症患者的生存率,因为这些患者机体中没有名为1p和19p的基因突变。研究者对来自全球的750名患者进行研究,将研究对象分为4组,分别为:1)单独放疗组;2)放疗和化疗同时进行组;3)先放疗后化疗治疗组;4)放疗和化疗同时进行,并且随后进行化疗的治疗组。
研究者指出,放疗后进行化疗(第三组和第四组)可以持续抑制患者机体肿瘤长达43个月,而仅进行放疗或两种疗法同时进行的患者机体肿瘤被抑制仅能持续19个月。放疗后化疗可以使得56%的患者存活5年,而化疗和放疗同时进行对患者的治疗效益目前研究者还不清楚。
研究发现放疗后给予药物替莫唑胺进行化疗可以有效减缓癌症的进展并且明显改善癌症患者的生存,这项临床试验可以改善当前研究人员进行间变性胶质瘤的治疗方法。英国癌症研究中心的研究者们就开展了替莫唑胺化学疗法的研究,其中包括实验室研究以及临床药物的开发和试验,而如今这种疗法可以用于治疗胶质母细胞瘤。(文章详见——ASCO 2016:放疗后进行化疗或可有效改善罕见脑瘤患者的生存率)
【6】 “以毒攻瘤”!首个“基因改造病毒”对抗脑瘤效果显著
6月1日发表在Science Translational Medicine上的一项研究揭示:一种实验性病毒疗法可以延长恶性胶质瘤患者的生命周期。
该项研究处于旨在评估安全性和耐受性的Ⅰ期临床试验阶段,患有恶性胶质瘤的病人在注入了一种工程病毒后,43位患者的生存期为13.6个月,相比之下,不接受该项疗法的患者生存期仅为7.1个月,提高了将近一倍。这是临床上,首次用数据证实了采用抗真菌药物的疗法不仅能杀死肿瘤细胞,而且还可以激活免疫系统攻击肿瘤细胞且保留健康细胞。
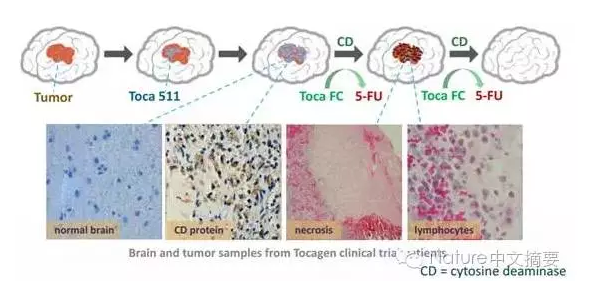
这种治疗方法的作用机制为:可注射的Toca 511经注射到病人体内后,感染活跃分裂的癌细胞,并且运送编码胞嘧啶脱氨酶的基因到这些癌细胞中。在肿瘤内部,Toca 511对癌细胞进行编程,产生胞嘧啶脱氨酶,从而为第二阶段治疗做好准备。
首先,研究者向积极分裂癌细胞中注射Toca 511病毒,该病毒上携带表达胞嘧啶脱氨酶的基因;然后,Toca 511在脑癌细胞中合成达胞嘧啶脱氨酶;最后,患者接受了一种叫做Toca FC的抗真菌药物,Toca 511引发的基因突变将Toca FC这样转化为抗癌药物5 -氟尿嘧啶(5-FU)。(文章详见——STM:“以毒攻瘤”!首个“基因改造病毒”对抗脑瘤效果显著)

【7】 Neurology:科学家发现与常见致死脑瘤相关的免疫基因
研究人员最近发现一组免疫相关基因可能会影响多形性成胶质细胞瘤病人的生存时间,相关研究结果在线发表在国际学术期刊Neurology上。多形性成胶质细胞瘤是神经胶质细胞形成的一种常见脑癌类型,这类肿瘤生长迅速,即使进行了手术,放疗以及化疗,患者平均生存时间也不超过两年。
在这项研究中,研究人员对297名脑部肿瘤患者的组织样本进行了研究,其中有127人患有成胶质细胞瘤,另外170人患有低级别胶质瘤,这也是一种由神经胶质细胞形成的肿瘤,但侵袭性弱于成胶质细胞瘤。研究人员经过基因组测序分析发现有322个免疫相关基因存在差异,其中有8个基因在成胶质细胞瘤中发挥重要作用,而这8个基因中有3个基因具有对抗成胶质细胞瘤的保护作用,而其他5个基因则会增加病人的死亡风险。研究人员根据这8个基因建立了用于风险分层的基因特征,并且发现定义为高风险的病人其死亡时间要早于低风险病人,这种分层方式也同样适用于低级别胶质瘤病人。
校正混杂因素后结果仍然相同。他们还对另外一个由536个成胶质细胞瘤样本组成的数据库进行了分析,也发现了相同的基因特征。(文章详见——Neurology:科学家发现与常见致死脑瘤相关的免疫基因)
【8】 治疗性抗癌疫苗与CAR-T疗法在脑瘤研究方面取得新突破
高级别神经胶质瘤(glioma)是最具侵袭性的脑癌之一,尽管手术、化疗和放疗能够让病情有所改善,但是这类患者存活超过5年的不到10%。3月2日,发表在Science Translational Medicine上的一项研究中,科学家们提出的新一代细胞免疫疗法或将为战胜脑癌带来希望。
细胞免疫疗法是通过注射治疗性抗癌疫苗刺激患者的免疫系统,使之能够攻击肿瘤。在这一研究中,鲁汶大学的科学家们将小鼠的脑癌细胞诱导成了一种特殊的死亡类型。随后,他们将这种垂死的癌细胞与树突状细胞一起培养。结果发现,垂死的癌细胞会释放危险信号,充分激活树突状细胞。研究显示,结合化疗,这种新型的细胞免疫疗法能够显着提高脑癌小鼠的生存率,几乎50%的小鼠被完全治愈。
近日,CAR-T疗法治疗实体瘤也取得了一项突破进展。发表在Cancer Immunology Research上的一项研究中,名古屋大学领导的研究小组发现,一种特殊的免疫细胞能够靶向肿瘤生长中的关键蛋白,帮助阻止脑癌发展。
成胶质细胞瘤是最常见、最具侵袭性的脑瘤之一,中数生存率仅14.6个月,5年生存率不到10%。PDPN是实体瘤发展过程中的一种关键蛋白。研究人员发现,注射他们设计的CAR-T细胞到79只免疫缺陷的小鼠中,成功阻止了其中60%的小鼠成胶质细胞瘤的生长。(文章详见——治疗性抗癌疫苗与CAR-T疗法在脑瘤研究方面取得新突破)
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











楼上这刷评论的?
99
学习了,很受益,谢谢分享,继续关注中!
103
不断进步,期望突破……
103
#研究进展#
56
#脑瘤#
78
放疗后进行化疗或可有效改善罕见脑瘤患者的生存率。
125
脊髓灰质炎病毒可治疗脑瘤。
63
脑瘤治疗重大突破,液态阿司匹林杀死癌细胞效率比化疗提高10倍。
80
大量研究表明,高程度教育会增加患脑瘤的风险,在大学学习至少3年的人比那些没有进入高等学府教育的人患神经胶质瘤的机率大。
56
多形性成胶质细胞瘤目前仍然是最致命的恶性脑瘤,而神经胶质瘤干细胞会促进治疗抵抗和肿瘤复发。
0