宫内节育器与生殖道感染的研究
2016-04-22 韩姹 薛凤霞 中国实用妇科与产科杂志
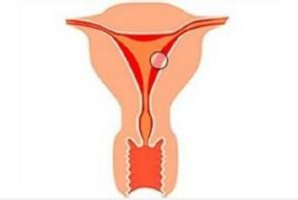
关于IUD操作前进行细菌性阴道病及STD的筛查必要性、IUD手术操作是否常规预防性应用抗生素以及应用IUD避孕妇女患PID处理的问题综述 宫内节育器(introuterine device,IUD)是我国育龄妇女的主要避孕措施。国家人口计生委调查发现,在2.3亿采用各种避孕措施的已婚育龄妇女中,有1.14亿妇女正在使用IUD,占49.79%。尽管已有文献资料显示,特别是对于性传播疾病
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










有收获
89
#生殖道#
49
#宫内节育器#
74
研究,结果如何?
131
文章不错
118
值得关注
138
学习了,目前很多这类研究
119
可以研究
89