Chest:NSCLC伴有脏层胸膜浸润(VPI)的改良病理T分期:来自中肿1055例≤3cm NSCLC病例分析
2021-12-24 yd2105 MedSci原创
研究表明,对于≤3cm NSCLC患者,PL1应该仍被定义为T1期而非T2期。同时在淋巴结阴性,≤3cm以及PL1的NSCLC患者中应避免术后辅助化疗。
脏层胸膜浸润(VPI)被认为是非小细胞肺癌(NSCLC)患者的不良预后因素。VPI的阳性将T1期增加至T2,从而IA期变成IB。对于IB期伴有VPI阳性患者,可建议术后辅助化疗。但是,VPI对于NSCLC患者预后的影响仍有争议。2008年,国际肺癌研究协会(IASLC)提出VPI病理标准,建议使用弹力纤维染色进行VPI诊断。根据标准胸膜侵犯分四个层次:PL0浅表侵入脏层胸膜弹力层;PL1,越过弹力层,但未侵入间皮层;PL2,侵犯脏层胸膜;PL3,侵犯壁层胸膜。对于肿瘤大小≤3cm患者,PL1和PL2被认为是T2期。但是PL1是否跟PL2一样对患者OS有影响?现有的研究结果仍存在矛盾。可能跟研究使用的方法诊断VPI有关,某些使用HE染色,某些使用弹力纤维染色。因此,来自中山大学肿瘤防治中心的杨浩贤教授团队开展了相关研究,目的是评估VPI对肿瘤大小≤3cm的NSCLC患者生存的影响。VPI诊断同时使用HE染色和弹力纤维染色。研究还提出了一种基于VPI的改良T分期,使分期更加准确。相关研究结果发表在Chest杂志上。
本研究共纳入1055例肿瘤大小≤3cm的原发NSCLC患者。组织学分型以腺癌为主(n=908, 86.1%)。以病理性I期居多(n=685, 64.9%)。PL1和PL2组的肿瘤比PL0组的更大(PL0 vs PL1: P<0.01; PL0 vs PL2: P=.042),PL1和PL2组患者比PL0组有更高的病理N分期(PL0 vs PL1: P<0. 01;PL0 vs PL2: P<0.01)。PL1组和PL2组的肿瘤大小类似(P=0.592)。此外,PL1组和PL2组的病理N分期、病理分期和辅助治疗类似。
824例患者诊断VPI为PL0, 133例患者诊断为PL1, 98例患者诊断为PL2。
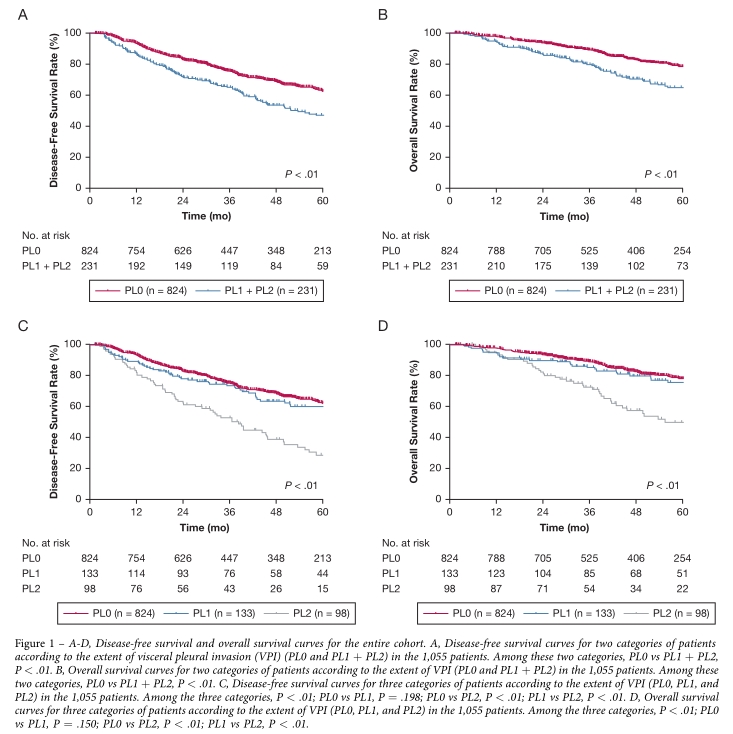
总体人群中位随访时间为49.4个月,范围为1.4 ~ 191.1个月。1055例患者中,随访期间有265例(25.1%)患者复发。复发类型仅局部复发49例(18.5%),局部复发合并远处转移57例(21.5%),仅远处转移159例(60.0%)。PL0、PL1和PL2患者的5年DFS率分别为62.6%、60.2%和28.8% (P<0.01),而相应的5年OS率分别为78.6%、74.4%和50.0% (P<0. 01)。
当PL1和PL2患者合并在一起时,这些患者的DFS和OS比PL0患者差(P<0.01)。然而,PL0, PL1,和PL2三组患者相比,无论是DFS (P=0.198)还是OS(P=0.150),PL0和PL1患者类似。但是PL2患者的预后较PL0和PL1患者的差(P<0.01)。
三组DFS和OS差异
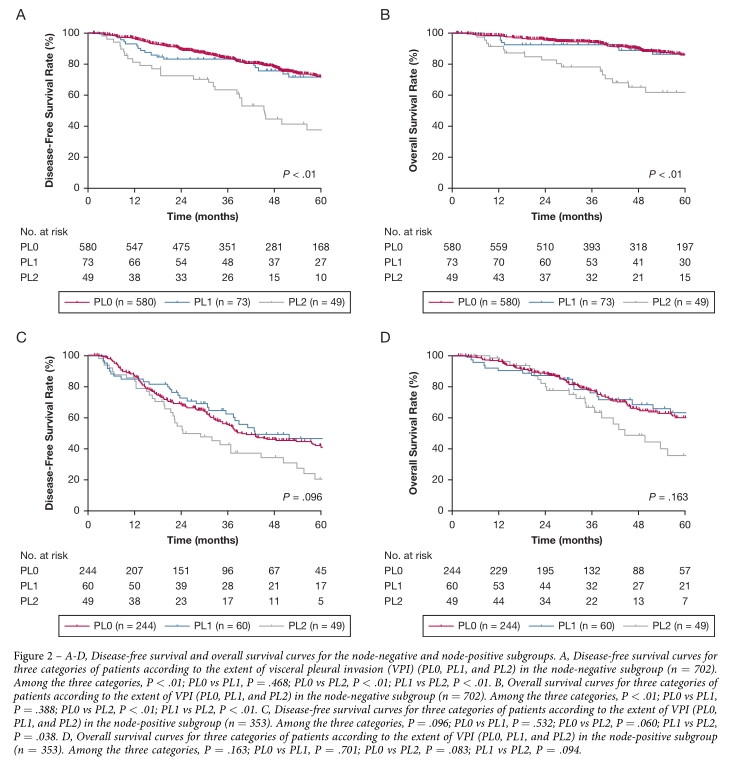
当只考虑淋巴结阴性患者时,数据再次表明PL0和PL1患者的长期生存类似(DFS: P=0.468;OS: P=0.388),但PL2患者的DFS和OS比PL0和PL1患者差得多(P<0.01)。然而,当仅考虑淋巴结阳性患者时,三组患者的长期生存类似。
淋巴结阴性和阳性分层三组的DFS和OS差异
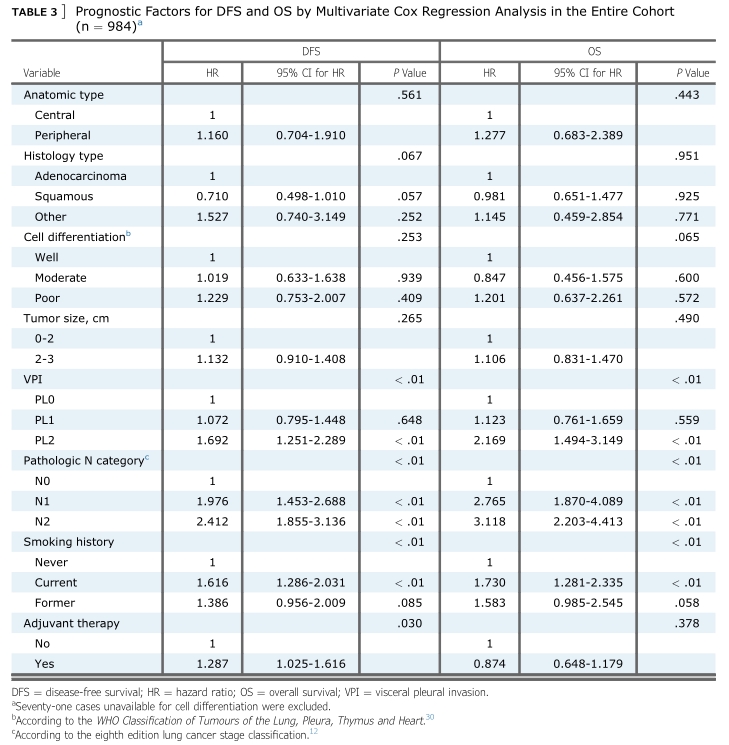
多因素分析发现,PL2(hazard ratio [HR], 1.692; 95% CI, 1.251-2.289; P <0.01),淋巴结阳性(N1: HR, 1.976; 95% CI, 1.453-2.688; P <0.01; N2: HR, 2.412; 95% CI, 1.855-3.136; P <0.01), 以及目前吸烟中(HR, 1.616; 95% CI, 1.286-2.031; P <0.01)是DFS不良独立预后因素。而PL2 (HR, 2.169; 95% CI, 1.494-3.149; P <0.01), 淋巴结阳性(N1: HR, 2.765;95% CI, 1.870-4.089; P <0.01; N2: HR, 3.118; 95% CI,2.203-4.413; P <0.01), 以及目前吸烟中(HR, 1.730; 95% CI, 1.281-2.335; P <0.01)是OS不良独立预后因素。
DFS和OS多因素分析
进一步分析,仅纳入N0患者时,研究显示PL2和较差细胞分化是DFS和OS不良独立预后因素。
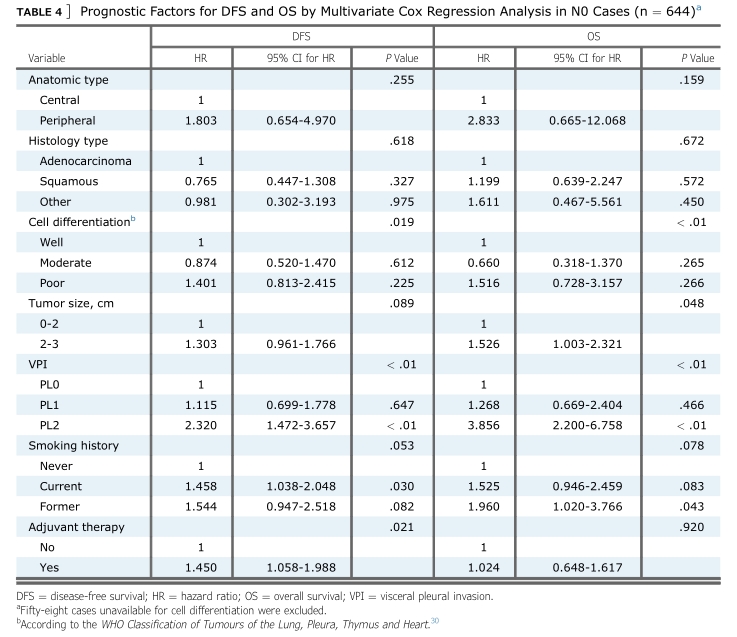
N0患者DFS和OS多因素分析
综上,研究表明,对于≤3cm NSCLC患者,PL1应该仍被定义为T1期而非T2期。同时在淋巴结阴性,≤3cm以及PL1的NSCLC患者中应避免术后辅助化疗。
原始出处:
Liang RB, Li P, Li BT, Jin JT, Rusch VW, Jones DR, Wu YL, Liu Q, Yang J, Yang MZ, Li S, Long H, Fu JH, Zhang LJ, Lin P, Rong TH, Hou X, Lin SX, Yang HX. Modification of Pathologic T Classification for Non-small Cell Lung Cancer With Visceral Pleural Invasion: Data From 1,055 Cases of Cancers ≤ 3 cm. Chest. 2021 Aug;160(2):754-764. doi: 10.1016/j.chest.2021.03.022. Epub 2021 Mar 18. PMID: 33745993; PMCID: PMC8449009.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Chest#
84
#胸膜#
81
#EST#
77
学习了
113