J Matern Fetal Neonatal Med:分娩途径对孕产妇分娩后并发症发病率的影响
2021-07-14 MedSci原创 MedSci原创
关于围产期(妊娠23 0/7-25 6/7周)最佳分娩途径的临床决策,很多文献都集中在新生儿风险上。事实上,在这些早孕期的常规剖腹产并没有被证明可以改善新生儿的死亡率或神经系统的结果。当前已知与分娩途
关于围产期(妊娠23 0/7-25 6/7周)最佳分娩途径的临床决策,很多文献都集中在新生儿风险上。事实上,在这些早孕期的常规剖腹产并没有被证明可以改善新生儿的死亡率或神经系统的结果。当前已知与分娩途径有关的新生儿风险是众所周知的,但是与分娩途径相关的孕产妇发病率的数据却非常少。近日,一项回顾性队列研究中,研究人员根据围产期妇女尝试的分娩途径对孕产妇的发病率进行了研究,研究结果已发表于J Matern Fetal Neonatal Med。

研究人员比较了围产期妇女尝试阴道分娩和计划中的剖腹产的产妇结果。重复分析以比较实际分娩方式(阴道分娩与剖腹产)的产妇结果。多变量泊松回归估计校正后的相对风险(aRR)和95%的置信区间(95%CI)。
结果显示,在678名接受围产期分娩的妇女中,558名(82.3%)和120名(17.7%)分别尝试了阴道分娩和计划中的剖腹产。在558名尝试阴道分娩的妇女中,411名(73.7%)实现了阴道分娩。与那些计划剖腹产的妇女相比,尝试阴道分娩的妇女患子宫内膜炎的可能性较小(3.1 vs. 15.0%;aRR 0.18,95%CI 0.09-0.35)。与计划剖腹产的妇女相比,尝试阴道分娩的妇女总住院时间短7天(P<0.001)。实际分娩方式的比较显示,与剖腹产相比,阴道分娩的妇女发热(2.9对7.9%;aRR 0.42,95% CI 0.20-0.90)、子宫内膜炎(0.5 vs. 12.4%;aRR 0.03,95% CI 0.01-0.13)和产妇血栓(0.2 vs. 3.0%;aRR 0.08,95% CI 0.01-0.93)的风险降低。与剖腹产相比,阴道分娩的产妇总住院时间缩短了3天(P < .001)。
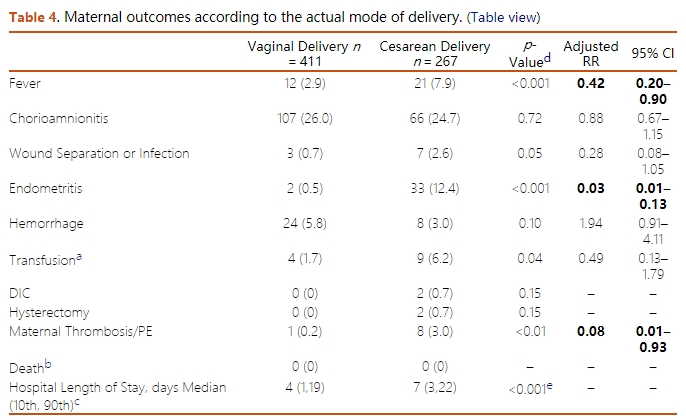
综上,大多数尝试阴道分娩的妇女(73.7%)实现了阴道分娩。与计划剖腹产的妇女相比,在妊娠23 0/7和25 6/7周之间尝试阴道分娩与产妇感染性发病率的风险降低有关。对于接受围产期分娩的妇女来说,决定分娩的途径是具有挑战性。我们的分析为在这些讨论中考虑风险和利益时提供了关于短期孕产妇风险的重要信息。
原始出处:
Tetsuya Kawakita, et al., Maternal morbidity by attempted route of delivery in periviable birth. J Matern Fetal Neonatal Med. 2021 Apr;34(8):1241-1248. doi: 10.1080/14767058.2019.1631792.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
90
#Neon#
81
#发病率#
92
#Nat#
87
#分娩#
97
#ATA#
0
#Med#
71