J Trauma Acute Care Surg:肠上皮细胞来源的外泌体触发创伤后免疫功能障碍
2017-12-03 MedSci MedSci原创
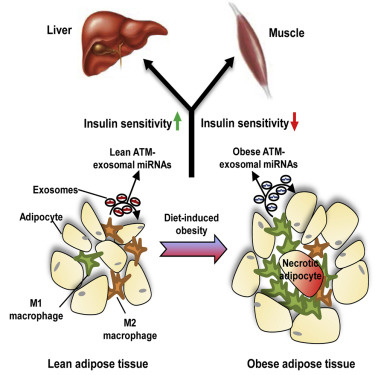
外泌体是作为免疫应答的内源性介质的细胞外囊泡。我们以前已经表明,在外伤/失血性休克(T/HS)后释放到肠系膜淋巴(ML)中的外泌体诱导巨噬细胞中促炎细胞因子的产生,并参与休克后急性肺损伤的发病机制。然而,ML外泌体的细胞来源及其在创伤后免疫应答中的作用仍不清楚。我们假设从受损肠上皮细胞(IECs)释放的外泌体通过改变树突细胞(DCs)(适应性免疫的关键调节剂)的功能来促进创伤后免疫功能障碍的发生。
外泌体是作为免疫应答的内源性介质的细胞外囊泡。我们以前已经表明,在外伤/失血性休克(T/HS)后释放到肠系膜淋巴(ML)中的外泌体诱导巨噬细胞中促炎细胞因子的产生,并参与休克后急性肺损伤的发病机制。然而,ML外泌体的细胞来源及其在创伤后免疫应答中的作用仍不清楚。我们假设从受损肠上皮细胞(IECs)释放的外泌体通过改变树突细胞(DCs)(适应性免疫的关键调节剂)的功能来促进创伤后免疫功能障碍的发生。
对雄性大鼠进行股动脉、颈静脉和ML导管的插管。开腹手术诱导T/HS,60分钟失血性休克,然后复苏。休克前和T/HS后收集ML以分离外泌体。通过流式细胞术评估从ML分离的外泌体的表面特征,以确定其细胞起源和表型变化。通过膜联蛋白V凋亡测定,共刺激分子的表达和对淋巴细胞的抗原呈递能力来评估ML外体对DC的免疫调节作用。
结果显示,从ML分离的外泌体高度表达CD63(外泌体标志物)和EpCAM(上皮细胞特异性标志物),表明它们来自IECs 。T/HS后ML外泌体免疫调节分子,如MHC II类分子和Fas配体,的表达显著增加。与T/HS后从ML分离的外泌体共培养后,DCs细胞的凋亡较休克前ML外泌体增加了2倍。此外,T/HS后 ML外泌体明显抑制LPS介导的DCs CD80和CD86的表达,并降低其诱导淋巴细胞增殖的抗原呈递能力。
综上所述,该研究结果表明,T/HS和复苏后,肠上皮细胞释放免疫调节性外泌体进入ML。 ML外泌体可能是创伤后免疫抑制导致DCs消耗和功能障碍的关键介质。
原始出处:
Kojima M, Costantini TW, et al., Gut Epithelial Cell-derived Exosomes Trigger Post-trauma Immune Dysfunction. J Trauma Acute Care Surg. 2017 Nov 21. doi: 10.1097/TA.0000000000001748.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
52
#Trauma#
49
#肠上皮细胞#
59
#创伤#
39
#Acute#
61
#功能障碍#
52
#免疫功能#
66
#上皮细胞#
44
学习一下谢谢分享
75
学习了受益匪浅
92