Front Oncol:新辅助化疗对卵巢癌伴有BRCA1/2不同突变状态患者的疗效
2022-02-04 yd2015 MedSci原创
研究表明,对于FIGO IIIB、IIIC和IV型卵巢癌患者伴有不同BRCA1/2生殖系突变状态,NAC-IDS并未对生存结果产生不利影响。
近期,山东大学附属医院团队在Frontiers in Oncology杂志上发表了一项研究成果,主要是评估新辅助化疗(NAC)+中间肿瘤细胞减灭术(interval debulking surgery,IDS)对比初次肿瘤细胞减灭术(primary debulking surgery,PDS)对卵巢癌伴有BRCA1/2不同突变状态患者的疗效。
共纳入322例 IIIB, IIIC, 和IV期卵巢癌患者,其中BRCA1/2突变(BRCAmut)患者112例,BRCA1/2野生型(BRCAwt)患者210例。BRCAmut患者和BRCAwt患者的中位年龄分别为52岁(34-79)和54岁(23-75),差异无统计学意义(p=0.439)。两组患者接受NAC的比例(35.7% vs. 32.9%, p=0.606)、FIGO分期(p=0.408)、诊断时最大原发肿瘤(p=0.753)、血清CA-25水平(p=0.430)也无统计学差异。
中位随访期为48.9个月[四分位数范围(IQR), 22.8 64.2]。无论BRCA1/2突变状态如何,NAC-IDS和PDS组的中位PFS(中位数:15.4 vs. 15.6个月,HR=0.85;p=0.211)或OS(中位数:57.1 vs. 64.7个月,HR=1.12;p = 0.486)都没有统计学差异。
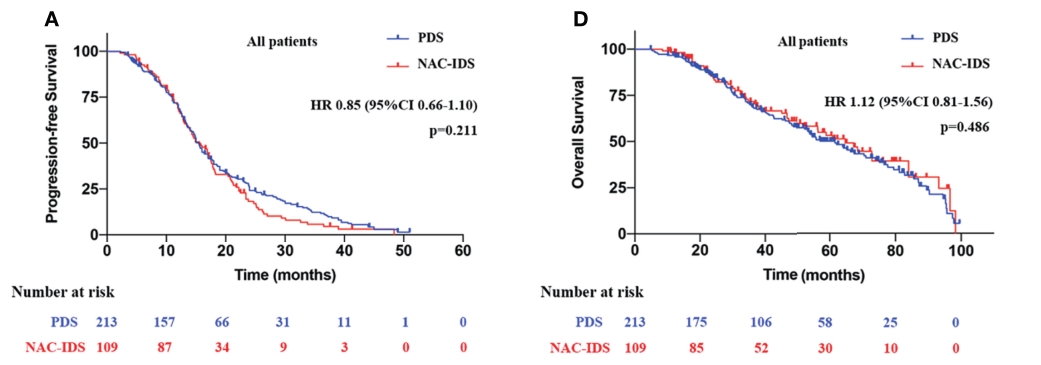
所有患者治疗的PFS和OS差异
进一步分析发现,BRCAmut患者中,NAC-IDS组的PFS较PDS组明显缩短(中位数,14.9 vs. 18.5个月,HR=0.59;p = 0.023);然而,OS无统计学差异(中位数,75.1个月vs 72.8个月,HR=0.93; p = 0.798)。BRCAwt患者中,NAC-IDS和PDS组的中位PFS(中位数,13.5 vs. 16.0个月,HR=1.05;p=0.781)和OS(中位数,54.0个月vs. 56.4个月,HR=1.23;p = 0.323)没有统计学差异。
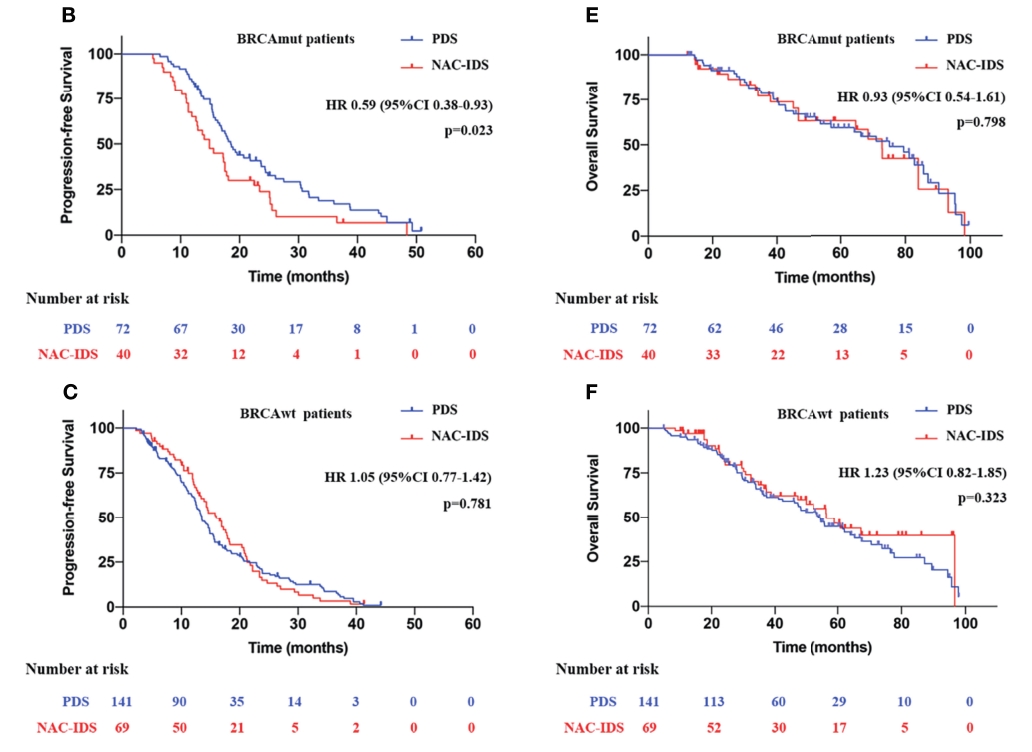
BRCA突变或野生型患者治疗的PFS和OS差异
所有患者中,PFS延长的预测因素有BRCA突变(p=0.007)、无残留病灶(p=0.003)和CA-125水平低(p=0.004);对于BRCAmut患者,预测因素有FIGO III期(p=0.020)、PDS (p=0.001)和无残留病灶(p=0.012);对于BRCAwt患者,低CA-125水平(p=0.011)、无残余病变(p=0.028)是延长PFS的预测因子。进一步的OS分析表明,无论患者的其他临床特征如何,PARP抑制剂是BRCAmut患者的独立预测因子(p=0.000);对于本研究中的所有患者,PARP抑制剂和没有残留病灶是OS延长的最强预测因素(PARP抑制剂,p=0.000;R0, p=0.036),结果在BRCAwt患者中是一致的(PARP抑制剂,p=0.000;R0, p=0.041)。
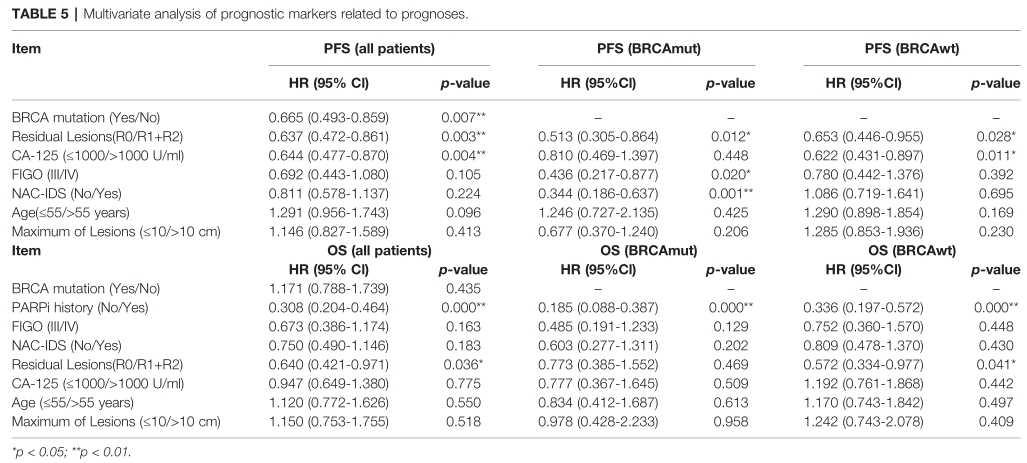
多因素分析
综上,研究表明,对于FIGO IIIB、IIIC和IV型卵巢癌患者伴有不同BRCA1/2生殖系突变状态,NAC-IDS并未对生存结果产生不利影响。
原始出处:
Fu M, Jin C, Feng S, Jia Z, Nie L, Zhang Y, Peng J, Wang X, Bu H and Kong B (2022) Effects of Neoadjuvant Chemotherapy in Ovarian Cancer Patients With Different Germline BRCA1/2 Mutational Status: A Retrospective Cohort Study. Front. Oncol. 11:810099. doi: 10.3389/fonc.2021.810099
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新辅助#
75
#Oncol#
78
很不错的研究,解决临床问题。
95
#BRCA1#
137
#BRCA1/2#
116
#BRCA#
107