AJOG:炎症因子预测早产胎膜早破(PPROM)胎儿神经系统情况
2015-02-20 Mechront译 MedSci原创
早产儿的一个主要不良妊娠结局是长期的神经系统发育不良,如大脑性麻痹。而前期有研究证实早产胎膜早破PPROM与胎儿神经系统发育不良有关。而母胎间炎症反应会导致母亲PPROM和胎儿神经系统发育不良。另外与胎儿胎盘炎症相关的细胞因子,不管有没有诱发感染,均会影响胎儿大脑发育。Armstrong-Wells J等人进行了一项前瞻性队列研究以探究母体和胎儿血样中不同的细胞因子标志物,能否反映胎盘炎
早产儿的一个主要不良妊娠结局是长期的神经系统发育不良,如大脑性麻痹。而前期有研究证实早产胎膜早破(PPROM)与胎儿神经系统发育不良有关。而母胎间炎症反应会导致母亲PPROM和胎儿神经系统发育不良。另外与胎儿胎盘炎症相关的细胞因子,不管有没有诱发感染,均会影响胎儿大脑发育。Armstrong-Wells J等人进行了一项前瞻性队列研究以探究母体和胎儿血样中不同的细胞因子标志物,能否反映胎盘炎症类型,以及对伴有PPROM出生的胎儿在6个月大小时的神经系统发育情况。
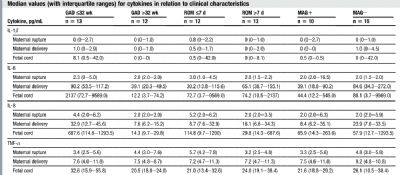
该研究共纳入25名PPROM女性,分别在破膜和分娩时,通过酶联免疫法检测血浆细胞因子(IL-1β,IL-6,IL-8,TNF-α)水平,同时抽脐血检测以上细胞因子指标。不同的胎盘病理会产生不同的细胞因子。胎儿出生后行头颅B超,且在早产儿矫正胎龄后的第6个月行神经系统检查。通过线性回归探究炎症预测因子与胎儿神经系统结局的关系且矫正出生时胎龄。
研究结果显示,胎盘胎儿面炎症时,母体生产时其血浆IL-6、IL-8增高,胎儿血浆中IL-1β、IL-6、IL-8和TNF-α均增高。不管出生时胎龄和出生时颅脑B超检查结果,胎盘胎儿面炎症和破膜到生产间歇时间过短与婴儿6个月时不良神经系统结局有关。
该研究表明,不管PPROM胎儿出生时颅脑情况如何,其神经系统发育不良与胎儿炎症有关。后期需要更多的纵向研究以充分验证结果,同时做出风险评估和干预策略。
原始出处:
Armstrong-Wells J, Donnelly M, Post MD, et al. Inflammatory predictors of neurologic
disability after preterm premature rupture of membranes. Am J Obstet Gynecol 2015;
212:212.e1-9.
下载:![]() nflammatory predictors of neurologic disability after preterm premature rupture of membranes..pdf
nflammatory predictors of neurologic disability after preterm premature rupture of membranes..pdf
本文是Medsci原创编译整理,欢迎转载!转载请注明来源并附原文链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PROM#
81
东西还是不错的。可以多学习
148
#神经系统#
98
#胎膜早破#
75
#PRO#
60