Front Immunol:来源于卵巢癌和卵巢囊肿的外泌体处理淋巴细胞其基因表达差异
2017-08-06 MedSci MedSci原创
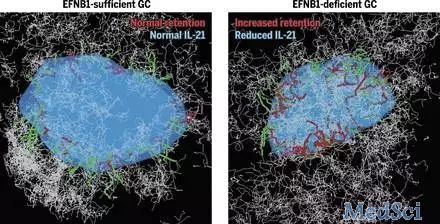
癌细胞可利用多种策略来逃避免疫防御,促进肿瘤的生长和血管的生成。作为一种新型的细胞间通讯方式,肿瘤来源的外泌体有助于肿瘤环境中淋巴细胞的聚集及介导。然而,外泌体作用于淋巴细胞的机制及关键分子目前尚不清楚。研究人员使用来源于卵巢癌及卵巢囊肿的外泌体处理健康人的外周血淋巴细胞,使用RT2 探查肿瘤炎症和免疫串扰PCR阵列筛选差异表达的基因。结果显示,共有26个基因表达上调(主要是促炎基因、免疫刺激和免
癌细胞可利用多种策略来逃避免疫防御,促进肿瘤的生长和血管的生成。作为一种新型的细胞间通讯方式,肿瘤来源的外泌体有助于肿瘤环境中淋巴细胞的聚集及介导。然而,外泌体作用于淋巴细胞的机制及关键分子目前尚不清楚。
研究人员使用来源于卵巢癌及卵巢囊肿的外泌体处理健康人的外周血淋巴细胞,使用RT2 探查肿瘤炎症和免疫串扰PCR阵列筛选差异表达的基因。
结果显示,共有26个基因表达上调(主要是促炎基因、免疫刺激和免疫抑制因子)和两个基因下调(抗原呈递HLA-A/B)。免疫印迹分析来自恶性腹水和良性卵巢囊肿腹腔冲洗液的淋巴细胞,表明NF-κB信号通路参与了恶性外泌体的免疫调节干扰。在使用芯片检测的28个差异表达基因中,使用实时PCR验证了卵巢癌(n=27)和卵巢囊肿(n=9)环境中淋巴细胞的11个。
总而言之,该研究结果表明,癌细胞分泌的外泌体在肿瘤微环境中可募集淋巴细胞,通过干扰素和NF-κB信号通路来抑制抗肿瘤免疫(IL10,Foxp3和HLA-A/B),增强肿瘤侵袭、血管生成和促炎细胞因子(如IL-6和VEGFA)的传播。这些结果阐明了淋巴细胞-癌细胞通过外泌体相互作用,且或可促进开发卵巢癌有效免疫治疗策略的开发。
原始出处:
Yujuan Li, Yang Yang, et al., Comparative Gene Expression Analysis of Lymphocytes Treated with Exosomes Derived from Ovarian Cancer and Ovarian Cysts. Front Immunol. 2017; 8: 607. Published online 2017 Jun 1. doi: 10.3389/fimmu.2017.00607.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#表达差异#
95
#卵巢囊#
73
#淋巴细胞#
67
#囊肿#
101
#基因表达#
60
学习了,谢谢分享
130
非常好的文章,学习了,很受益
137
学习了,谢谢
134
henhao
136