J ImmunoTherapy Cancer:质谱技术直接检测肿瘤新生抗原,癌细胞无所遁形!
2019-11-25 Blake 转化医学网
导 读:肿瘤细胞表面独特的生物标志物将肿瘤细胞和正常细胞区分开来,免疫系统可根据这些标志物特异性识别肿瘤细胞,这也是很多免疫疗法的基础。
近日,伦敦癌症研究所和瑞士洛桑路德维希癌症研究所的研究人员通过质谱技术,直接测量了晚期结直肠癌患者衍生的类器官(Patient derived organoids,PDOs)的新生抗原数量,发现晚期结直肠癌细胞表面的新生抗原比计算机预测的要少得多,这也解释了当前免疫疗法对大多数晚期结直肠癌疗效不佳的原因。这一发现揭示了免疫治疗所面临的挑战,但同时也为个性化肿瘤疫苗的研制铺平了道路。
肿瘤细胞有大量的基因突变,由此产生变异蛋白,并被主要组织相容性复合体呈递于细胞表面,这些生物标志物也称为新生抗原。新生抗原的检测大大加速了肿瘤患者个体化免疫治疗的发展,比如用于预测患者对免疫治疗的反应,或者据此设计个体化肿瘤疫苗。
通常而言,肿瘤细胞新生抗原的发现主要通过对测序数据的分析,即首先对肿瘤进行高通量测序,然后通过计算机对序列突变和白细胞抗原配型进行解析。但该研究发现,晚期结直肠癌患者细胞表面的新生抗原比计算机预测的要少得多。
患者衍生的类器官(Patient derived organoids,PDOs)是一种具有很好预测能力的临床前模型,是将患者肿瘤在体外3D培养成“微型器官”,PDO模型具有很多其它临床前模型如PDX模型(人源肿瘤异种移植模型,Patient-Derived tumor Xenograft)所没有的优势。
尤其是,直接从患者身上采集的样本会有一些正常组织细胞,导致严重影响新生抗原的分析。而PDO则没有其他类型细胞的污染,这大大降低了对新生抗原的分析难度。
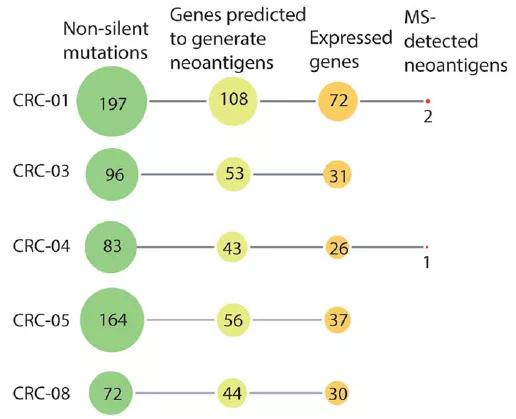
研究人员分析了5名结直肠癌患者的PDO,从中发现了可能产生新生抗原的612个基因突变。然而,他们仅仅检测到了3个新生抗原,远低于计算机预测的结果。
对5名结直肠癌患者PDOs的新生抗原计算机预测和质谱检测
蛋白质谱技术已广泛应用于蛋白质的鉴定测序等领域,在该研究中,首次成功利用基于质谱的免疫蛋白组技术(MS-based immunopeptidomics)直接测量了微卫星稳定PDO癌细胞表面的新生抗原。同时,他们还用IFN-γ和靶向药物曲美替尼对PDO进行了处理,以测试能否增加癌细胞表面新生抗原的数量。
前期研究表明,IFN-γ和曲美替尼可以增加新生抗原的表达,但在该研究中并没有发现这种效果。
这项新技术使研究人员能够直接检测新生抗原,而不必依赖于计算机预测,大大增加了新生抗原检测的准确性。
虽然基于质谱的免疫蛋白组技术有一定的限制,比如有限的灵敏度可能导致无法检测部分新生抗原,但该研究结果表明采用基于质谱的免疫蛋白组技术对结直肠癌PDOs新生抗原检测是可行的。
晚期结直肠癌患者的新生抗原数量远远少于预测,导致难以被免疫免疫细胞识别。这一发现揭示了免疫治疗所面临的挑战,但同时也为个体化肿瘤疫苗的设计铺平了道路。
原始出处:
Alice Newey et al. Immunopeptidomics of colorectal cancer organoids reveals a sparse HLA class I neoantigen landscape and no increase in neoantigens with interferon or MEK-inhibitor treatment, Journal for ImmunoTherapy of Cancer (2019).
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ERA#
72
#质谱技术#
75
#癌细胞#
64
#质谱#
118
#抗原#
73