Hypertension:青年时期血清尿酸变化轨迹与中年心血管疾病事件
2021-06-19 MedSci原创 MedSci原创
青年期血清尿酸升高轨迹与中年期CVD事件相关,这种关联可以用暴露期间的血压水平进行解释。
血清尿酸水平已被证明与中年或老年人发生心血管疾病 (CVD) 事件的风险相关。然而,青年时期的血清尿酸盐变化轨迹及其与CVD事件之间的关联尚未得到充分研究。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员收集了3563名CARDIA(年轻成人冠状动脉风险发展)研究参与者(平均年龄为25.1±3.6 [基线时为18-30岁,第0年,1985-1986 年];46.3%为黑人;56.1%为女性)的血清尿酸测量值 。
研究人员采用SAS PROC TRAJ确定了性别特异性的血清尿酸变化轨迹。研究人员估计了从20次评估到2017年期间发生的CVD事件(冠心病、心力衰竭和卒中)风险比。研究人员按性别确定了3个血清尿酸变化轨迹,包括低稳定 (n=1251)、中稳定 (n=1761) 和高增长 (n=551)。
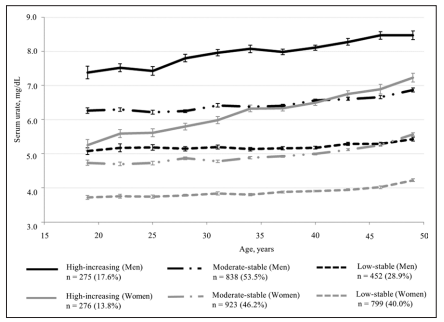
血清尿酸的变化轨迹
在中位10.6年的随访期间,共发生了157起CVD事件。与低稳定轨迹组相比,高增长组的参与者患CVD的风险高出2.89倍(95%CI为1.88-4.43)。在调整了青年时期的血压水平后,这种关联有所减弱。
总之,青年期血清尿酸升高轨迹与中年期CVD事件相关,这种关联可以用暴露期间的血压水平进行解释。
原始出处:
Nagisa Morikawa.et al.Serum Urate Trajectory in Young Adulthood and Incident Cardiovascular Disease Events by Middle Age: CARDIA Study.Hypertension.2021.https://doi.org/10.1161/HYPERTENSIONAHA.121.17555
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#变化轨迹#
59
#PE#
47
#TENS#
51
不错的文章
84
#血清尿酸#
62
#血管疾病#
53
#Hypertension#
53
好文
93