European Radiology:静脉注射碘造影剂对急性肾损伤患者真的有害吗?
2022-01-11 shaosai MedSci原创
长期以来,对比剂诱导的急性肾损伤(CI-AKI)被认为是暴露于碘化对比剂(ICM)患者的主要并发症,与死亡风险的增加以及潜在的慢性肾脏疾病(CKD)的加速发展相关。

长期以来,对比剂诱导的急性肾损伤(CI-AKI)被认为是暴露于碘化对比剂(ICM)患者的主要并发症,与死亡风险的增加以及潜在的慢性肾脏疾病(CKD)的加速发展相关。对CI-AKI风险的担忧阻碍了ICM在高危患者中的应用,而这些患者本来可以从ICM管理的诊断准确性改善中获益,并可能因此导致疾病诊断和治疗的延误。因此,临床上迫切需要确定接受造影剂增强的患者出现临床意义上的肾毒性和其他不良后果的真正风险,从而在平衡ICM应用带来的益处和潜在的不良影响时做出正确的临床决定。
在过去的十多年里,静脉注射(IV)ICM的肾毒性一直受到质疑,并且有报道称ICM暴露后急性肾损伤(AKI)的发生率被明显高估。
近日,发表在European Radiology杂志的一项研究探讨了ICM对接受造影剂增强CT扫描的住院AKI患者的肾功能恶化、肾脏替代治疗(RRT)诱导和死亡率的影响,并与接受非增强CT扫描的AKI患者进行了比较,为住院AKI患者的静脉注射(IV)ICM提供临床证据并指导临床实践。
本项回顾性研究评估了2015年1月至2019年12月期间,在AKI诊断后7天内接受造影剂增强或非增强CT扫描的成人住院患者,并进行了倾向性评分匹配。对照组和非对照组在CT扫描后7天和30天的结果进行了比较。还对按AKI诊断时的SCr水平、CT扫描的次数和时间分层的患者以及CT扫描前没有慢性肾脏疾病或RRT要求的患者进行了额外的分析。
在1:1的倾向性评分匹配后,总共产生了1172对,其中暴露于ICM的1336例,未暴露的2724例。两组之间的结果没有发现明显差异。DRF,7.8% vs 9.0%(OR0.83,95%置信区间(CI)0.62-1.11),30天内5.1% vs 5.4%(OR 0.93,95%CI 0.64-1.34);新的RRT诱导,2.3% vs 3.3%(OR 0.72,95%CI 0. 43-1.18),30天内4.2% vs 4.5%(OR 0.95,95%CI 0.64-1.41);死亡率,7天内3.9% vs 4.8%(OR 0.83,95%CI 0.56-1.22),30天内9.0% vs 10.2%(OR 0.88,95%CI 0.68-1.15)。子集分析显示了类似的结果。
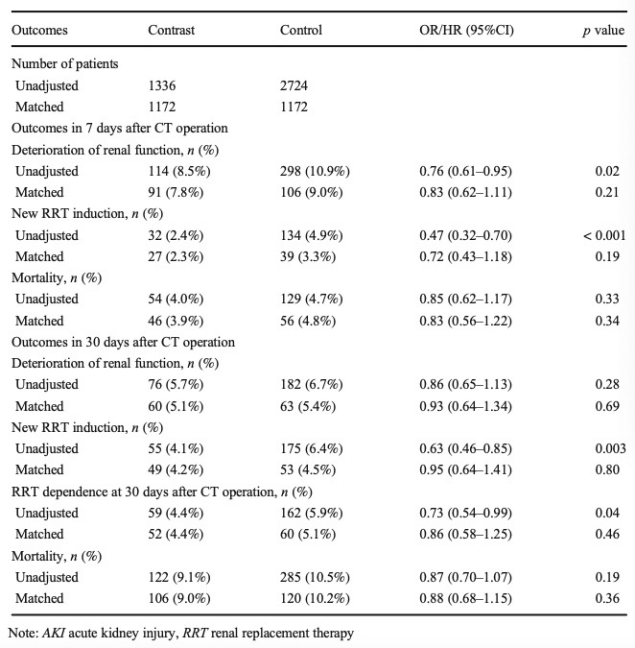
表 倾向性评分匹配前后的住院AKI患者的情况。
本研究表明,在住院的AKI患者中,静脉注射ICM的肾毒性很小。如果临床评估认为ICM对住院的AKI患者有益,则不应过分避免静脉注射ICM,以避免延误病情的诊断及评估。
原文出处:
Ping Yan,Ning-Ya Zhang,Xiao-Qin Luo.Is intravenous iodinated contrast medium administration really harmful in hospitalized acute kidney injury patients: a propensity score-matched study.DOI:10.1007/s00330-021-08192-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
65
#静脉#
66
学习了
65
#损伤#
52
#静脉注射#
70
#造影#
52
#静脉注射碘造影剂#
69