SCI REP:如何克服癌症治疗的抵抗性?科学研究有新发现!
2017-04-28 枫丹白露 来宝网
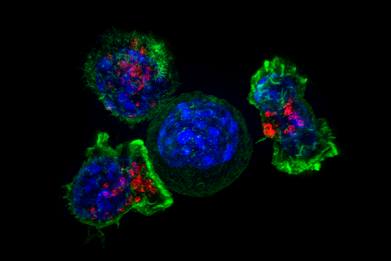
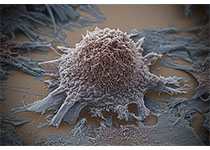
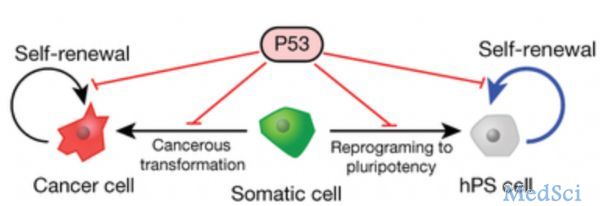
牛津大学和莫菲特癌症研究中心合作的克利夫兰诊所研究人员已经证明了这样一个理论,虽然对癌症靶向治疗的耐受和抵抗确实是一个持久的目标,但有机会克服抵抗性的发展。虽然需要更多的研究,但研究人员认为理解和预测肿瘤抵抗可能会转化为临床环境中的其他治疗方案。随着癌细胞发展而产生的治疗抵抗力是今天靶向癌症治疗的主要限制之一。在这一进程中,癌细胞不仅改变了对用于治疗癌症的药物的反应,而且改变了许多其他药物。在某些
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新发现#
56
#抗性#
58
#癌症治疗#
71
谢谢分享,药物假期
78
学习了,谢谢作者分享!
74