Lancet:从临床试验到临床实践,看真实世界中GLP-1RA的心血管获
2020-03-30 idiabetes idiabetes
2型糖尿病(T2DM)患者往往合并多重心血管危险因素,半数以上糖尿病患者的死亡与动脉粥样硬化性心血管疾病(ASCVD)密切相关。
2型糖尿病(T2DM)患者往往合并多重心血管危险因素,半数以上糖尿病患者的死亡与动脉粥样硬化性心血管疾病(ASCVD)密切相关。以往多项新型降糖药物GLP-1受体激动剂(GLP-1RA)的心血管安全性评价研究(CVOT)证实其具有心血管获益。那么在真实世界中,这一获益是否仍然存在?2019年发表在Lancet Diabetes Endocrinol 上的一项注册登记队列研究首次对比了利拉鲁肽与DPP-4抑制剂在真实世界中对T2DM患者心血管结局影响,在实际临床实践中再次验证了利拉鲁肽的心血管获益。
研究背景
自2008年美国FDA公布《治疗2型糖尿病新药的心血管风险评价指导原则》,要求未上市的降糖药物进行心血管安全性评价。随后上市的新型降糖药如DPP-4抑制剂、胰高GLP-1RA、SGLT2抑制剂均相继完成了其心血管结局研究。其中GLP-1受体激动剂利拉鲁肽在其多国、多中心、随机、双盲、安慰剂对照的心血管安全性评价研究(CVOT)LEADER研究中,被证实具有心血管获益。与安慰剂相比,在标准治疗基础上利拉鲁肽可使伴有心血管疾病或心血管高危的2型糖尿病患者的主要不良心血管事件(MACE:包括心血管死亡、非致死性心肌梗死、非致死性卒中复合终点)风险显著下降13%(P=0.01),心血管死亡风险显著降低22%(P=0.007),且不增加因心衰住院风险[1]。LEADER研究使利拉鲁肽成为首个被证实具有明确心血管获益的GLP-1类药物。
而利拉鲁肽在广泛人群及真实世界的临床实践中是否仍然具有心血管获益仍然未知。同时,也缺乏与活性药物针对心血管结局的对比研究。
研究设计与方法
这是一项注册登记队列研究,采用丹麦和瑞典国家注册机构2010年1月1日至2016年12月期间的数据,比较了GLP-1受体激动剂利拉鲁肽与活性药物DPP-4抑制剂对2型糖尿病患者的主要心血管不良事件风险的影响。
该研究纳入在基线时已使用二甲双胍的2型糖尿病患者,一组使用利拉鲁肽,另一组使用DPP-4抑制剂,按年龄、性别和倾向评分1:1匹配。主要终点是主要心血管事件,包括心肌梗死、卒中和心血管死亡的复合终点。其他终点包括主要复合终点的各组分,心力衰竭,全因死亡以及扩展的主要心血管事件结局,包括其他缺血性心脏病,冠状动脉血运重建和周围动脉疾病的复合终点。亚组分析按照国家(丹麦或瑞典)、性别(女性或男性)、年龄组(<65岁或≥65岁)、主要心血管疾病史和研究基线时胰岛素的使用情况分别进行。
研究人群包括2010年1月1日至2016年12月31日丹麦和瑞典35~84岁开始使用利拉鲁肽或DPP-4抑制剂治疗的所有患者。在研究开始前任何时候曾使用过任何GLP-1受体激动剂或DPP-4抑制剂的患者被排除在外。为了增加获取新发重大心血管事件的可能性并减少近期急性疾病的影响,在开始治疗前30天内入院的所有患者也将被排除在研究之外。
主要结果
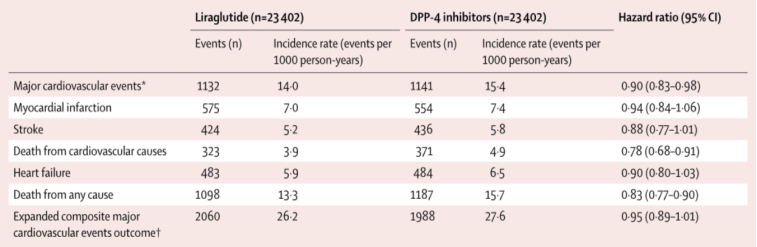
该研究共有23402例使用利拉鲁肽的患者匹配23402例使用DPP-4抑制剂的患者。平均随访时间3.3年(标准差2.0),其中共有1132例使用利拉鲁肽的患者发生了主要心血管不良事件(发生率14.0/1000患者·年);DPP-4抑制剂的使用者中共有1141例患者发生主要心血管不良事件(发生率15.4/1000患者·年)。
相对于DPP-4抑制剂,利拉鲁肽可降低主要心血管不良事件风险达10%(HR=0.90,95%CI:0.83~0.98)(图1)。对于既往有主要心血管疾病史的患者,相比DPP-4抑制剂,利拉鲁肽能降低此类人群19%的主要心血管不良事件风险(HR=0.81,95%CI:0.71~0.92)。而对于既往无心血管病史的患者,两种治疗方式对于主要终点的影响无显著差异(HR=0.96,95%CI:0.86-1.06,异质性检验P=0.057)。
与DPP-4抑制剂相比,利拉鲁肽显著降低心血管死亡风险(HR=0.78, 95%CI:0.68~0.91)和全因死亡风险( HR=0.83,95%CI:0.77~0.90) (表1);在心衰(HR=0.90,95%CI:0.80~1.03)或扩展的主要心血管事件结局(HR=0.95,95%CI:0.89~1.01)方面,二者无显著差异。
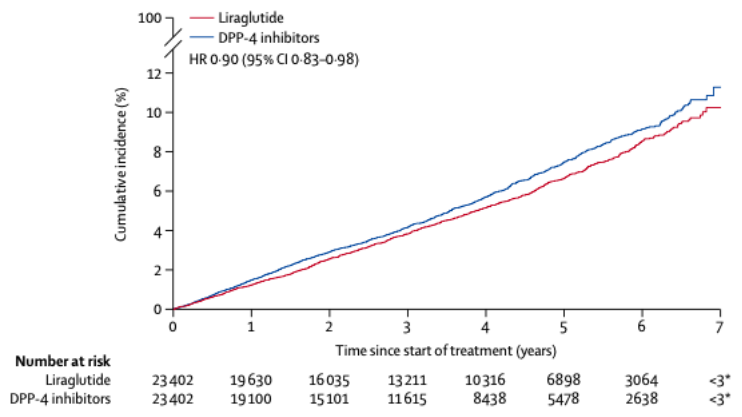
图1:与DPP-4抑制剂相比,利拉鲁肽显著降低主要心血管不良事件风险
表1:利拉鲁肽与DPP4抑制剂对心血管结局影响
研究结论
该研究在真实世界环境中首次将利拉鲁肽与活性药物DPP-4抑制剂针对心血管结局进行了比较。研究结果显示与DPP-4抑制剂相比,利拉鲁肽显著降低了主要不良心血管事件的发生风险,且在既往有心血管病史的患者中,其心血管获益更为显著。该研究结果与既往利拉鲁肽的大型随机对照心血管结局研究——LEADER研究结果一致,从临床试验到临床实践,再次验证了利拉鲁肽的心血管获益。
原始出处:
Svanström H, et al. Use of liraglutide and risk major cardiovascular events: a register-based cohort study in Denmark and Swede. Lancet Diabetes Endocrinol. 2019 Feb;7(2):106-114.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
59
#GLP-1R#
60
#真实世界#
46
#临床实践#
46
#GLP-1#
60
#GLP-1RA#
64