 infectiousdiseaseadvisor
infectiousdiseaseadvisor
被称为 “白色瘟疫”的肺结核(Tuberculosis, TB)大家并不陌生,是由结核杆菌感染引起的疾病,通常造成肺部感染,同时也会感染身体其它各系统。TB作为一种古老的疾病,已有上千年。1973年,湖南长沙马王堆汉墓出土的2100年前的女尸身上发现左上肺门均有结核病灶。
TB的流行演变可以分为三个时期,1882年结核杆菌被发现以前、1882-1945年抗TB药物广泛应用之前以及1945年至今现代化学疗法普及之后。
鉴于缺乏对结核病病原体的检测,且不能保证永久治愈肺部感染,WHO一般建议对标准疗法有反应的患者治疗时长至少6个月,对于耐药性结核病患者治疗时长不少18个月。也就是说,患者必须长时间每天服用四种以上抗生素,部分患者由于长期用药不可避免地出现听力丧失或者肝肾损伤等副作用。因此,缩短治疗时间是医学界一直在攻克的难题。
今年2月19日,德国肺脏研究中心(DZL)与德国感染研究中心(DZIF)合作的研究团队在《欧洲呼吸杂志》(European Respiratory Journal)发表的研究首次在肺结核患者中发现可以用于指导肺结核个体治疗时间的新的生物标志物。这将决定患者是否可以安全地提前结束疗程。
 Prediction of anti-tuberculosis treatment duration based on a 22-gene transcriptomic model. European Respiratory Journal, 2021; 2003492 DOI: 10.1183/13993003.03492-2020
Prediction of anti-tuberculosis treatment duration based on a 22-gene transcriptomic model. European Respiratory Journal, 2021; 2003492 DOI: 10.1183/13993003.03492-2020
为了识别这种个体生物标记,DZIF内的科学家建立了五个不同的肺结核患者队列,包括非耐药性和耐药性肺结核。临床和微生物学数据,以及用于RNA转录组分析的全血在整个治疗过程中按预定的时间点收集。治疗结果按TBNET标准确定(6个月培养状态/1年随访)。在一个涉及机器学习算法的多步骤过程中开发了一个全血RNA治疗结束模型,以确定假设的个人治疗结束时间点。
德国鉴定队列(DS-和MDR-GIC)招募了50名药物敏感(DS)肺结核患者和30名MDR肺结核患者,德国验证队列(DS-和MDR-GVC)招募了28名DS肺结核患者和32名MDR肺结核患者,罗马尼亚验证队列(MDR-RVC)招募了52名MDR肺结核患者。从DS-和MDR-GIC数据中推导出一个22个基因RNA模型,该模型定义了与治愈相关的治疗结束时间点。该模型优于其他已发表的标志物,能够准确预测DS-GVC患者的临床结果(AUC=0.94[95%CI:0.9-0. 98]),并提示MDR-GIC(平均减少218.0天,34.2%)、MDR-GVC(平均减少211.0天,32.9%)和MDR-RVC(平均减少161.0天,23.4)中的肺结核患者可能通过更短的治疗时间实现治愈。
研究人员从成千上万的基因中,鉴定出22个其活性与疾病进程相关的基因,这22个基因的RNA产生可以表示患者是否已经治愈。到目前为止,没有其他已发表的转录组标记物显示出可比的特性。
Borstel研究中心临床主任,研究负责人Christoph Lange表示:“治疗时间的个性化是结核病精准医学道路上的重要里程碑。” 该研究的重要价值在于,生物标志物指导下的治疗管理可以大幅缩短许多MDR-TB患者的治疗时间。下一步,研究人员计划在DZIF进行前瞻性研究,希望这样,耐多药结核病患者平均可以节省大约三分之一的治疗,这对患者来说,是极其有益的。
据世界卫生组织(WHO)2019年公布的数据显示,结核病是全球十大死因之一,也是单一传染病致死人数最多的疾病(自2007年以来排名高于艾滋病)。全球约有1000万人患病,死亡人数高达120万。
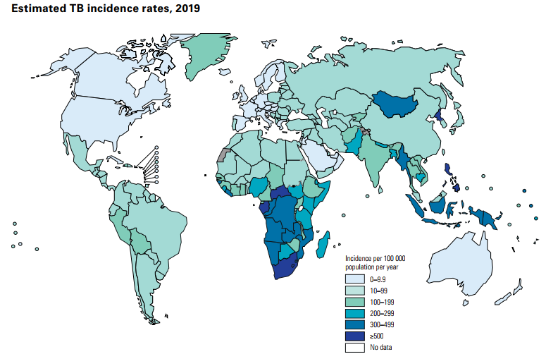
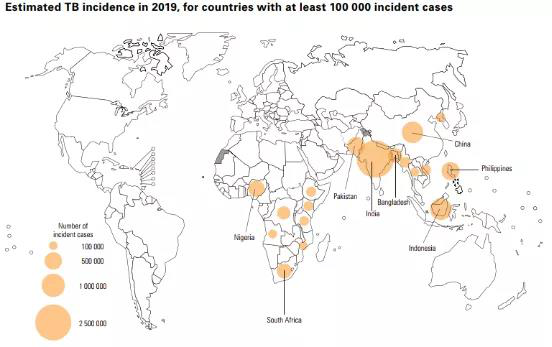 2019年结核病>10万的国家和地区tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
2019年结核病>10万的国家和地区tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
事实上,自二战后,各国坚持严格实施现代结核病控制策略,肺结核发病有所下降。然而,20世纪90年代末开始,由于对TB疫情控制的松懈、移民和难民增加、HIV感染与AIDs流行以及多耐药结核病例增加,全球TB疫情却有所回升。
2017年柳叶刀子刊发表的一项研究数据中显示,预测到2040年,俄罗斯近三分之一的结核病病例(32.5%)将是多药耐药性;在印度12.4%为多药耐药性;菲律宾为8.9%;南非为5.7%。这四个国家中将有十分之一的多药耐药结核病例具有广泛耐药性。
该研究预测,耐药菌株将导致耐药结核病例的减少-从2000年的约30%的多药耐药结核病例减少到2040年的20-25%,以及80%的广泛耐药病例抗药性疾病在2000年增加到2040年的50%。
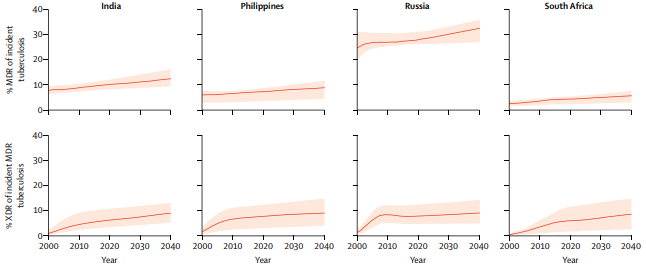 2000-2040年俄罗斯、印度、菲律宾和南非多药耐药性肺结核增长情况Estimating the future burden of multidrug-resistant and extensively drug-resistant tuberculosis in India, the Philippines, Russia, and South Africa: a mathematical modelling study. The Lancet Infectious Diseases, 17(7), 707–715. doi:10.1016/s1473-3099(17)30247-5
2000-2040年俄罗斯、印度、菲律宾和南非多药耐药性肺结核增长情况Estimating the future burden of multidrug-resistant and extensively drug-resistant tuberculosis in India, the Philippines, Russia, and South Africa: a mathematical modelling study. The Lancet Infectious Diseases, 17(7), 707–715. doi:10.1016/s1473-3099(17)30247-5
就我国来说,尽管近年来结核病防控取得了显著成就,但形势仍不容乐观,据世界卫生组织统计, 中国每年新发结核病患者数量多达90万, 新发耐多药结核病患者 7万(2018年数据)。正如前文所说,我国是全球30个结核病高负担国家之一,活动性肺结核病人数居世界第二位。根据《2010年全国第五次结核病流行病学抽样调查报告》显示,我国结核疫情现状可以用四个“高”进行总结:感染率高(44.5%)、患病率高(367/10万)、耐药率高(18.6/10万)且死亡率高(9.8/10万)。
多重耐药性结核病(MDR-TB)是指结核菌同时对两种最有效的第一线药物(利福平和异烟肼)具抗药性。某些情况下,还能出现广泛耐药性结核病,即对三种以上或六类最为有效的二线抗结核药物没有反应。
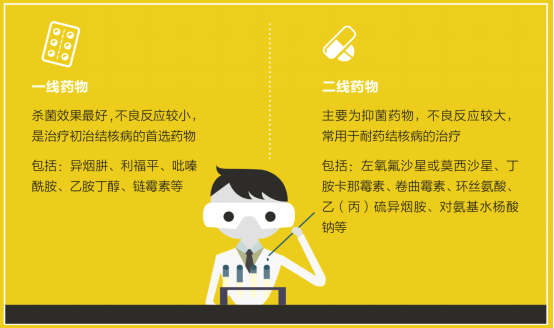 肺结核一线药物与二线药物区别,北京胸科医院结核病防治手册
肺结核一线药物与二线药物区别,北京胸科医院结核病防治手册
尽管大多数肺结核可被治愈,但耐药结核病的比例依然较高,据WHO的调查显示,几乎在全球各个国家均已发现耐药结核病,82%为多重耐药结核病(定义为对利福平和异烟肼同时耐药)。2016年有45个国家至少发生1000起耐药结核病病例,其中印度(25%),中国(12%)和俄罗斯(10%)几乎占全球总数的一半。逾九成国家有广泛耐药结核病的病例。仅2017年,有55.8万利福平耐药新发病例,其中82%是耐多药患者。为此,一般建议如果对检出MDR-TB的患者使用最少四种有效的抗生素进行为期18到24个月的治疗。
目前,多数耐多药和广泛耐药结核病患者需要联合使用8种以上抗生素,疗程为18个月以上,但治疗的成功率却并不高。WHO曾报告估计,广泛耐药结核病的治疗成功率约为39%,耐多药结核病的成功率约为56%。
自1940年代首次发现一种有效的抗结核抗生素以来,结核病领域的进步就一直很缓慢。而结核病患者感染了对现有药物有抗药性的结核菌株,治疗选择就非常有限。
此前,由结核病联盟(TB Alliance)组织的抗击耐药-创新结核化疗方案会议中提出了一种抗结核新药物化疗方案全口服组合疗法,由贝达喹啉、Pretomanid、利奈唑胺组成,即“BPaL”方案,BPaL的疗效在一项名为Nix-TB的关键临床试验中得到了证明。相关结果发表在《新英格兰医学》(NEJM)上。
 Treatment of Highly Drug-Resistant Pulmonary Tuberculosis. N Engl J Med. 2020 Mar 5;382(10):893-902.doi: 10.1056/NEJMoa1901814.
Treatment of Highly Drug-Resistant Pulmonary Tuberculosis. N Engl J Med. 2020 Mar 5;382(10):893-902.doi: 10.1056/NEJMoa1901814.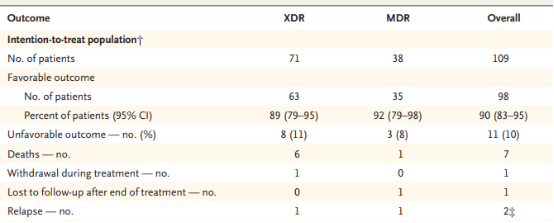 Treatment of Highly Drug-Resistant Pulmonary Tuberculosis. N Engl J Med. 2020 Mar 5;382(10):893-902.doi: 10.1056/NEJMoa1901814
Treatment of Highly Drug-Resistant Pulmonary Tuberculosis. N Engl J Med. 2020 Mar 5;382(10):893-902.doi: 10.1056/NEJMoa1901814
对于耐药性肺结核,新药的生产无疑给了人们一些希望,但在现有情况下,如果可以明确治疗终点时间,就可以大幅降低耐药性肺结核患者的治疗时间。在2019年的一项新研究中,加州大学洛杉矶分校戴维·格芬医学院团队报告称,可以通过使用一种名为“人工智能-抛物线反应面”的方法来大大减少耐药性肺结核治疗时间。众所周知,各个药物的协同作用比其各自效力的总和更有效,此数据分析方法就是确定哪些药物组合可以协同工作。
研究人员在数十亿种可能的药物和剂量组合中快速识别三种或四种药物组合,从而显著缩短了TB治疗的持续时间。这些方案既适用于药物敏感性结核病,也适用于大多数耐药结核病,并且比目前的标准治疗速度快五倍。需要提出的是,该方法仅用于细胞培养以及结核病小鼠模型,尚无人类试验。
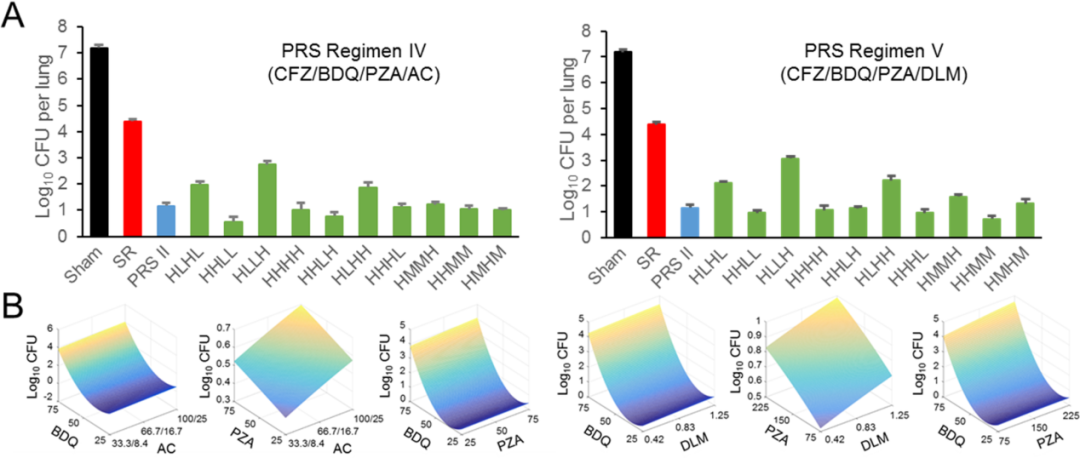 人工智能支持的抛物线反应面平台可识别由已获批药物组成的超快速近乎通用的结核病药物治疗方案。Artificial intelligence enabled parabolic response surface platform identifies ultra-rapid near-universal TB drug treatment regimens comprising approved drugs. PLOS ONE, 14(5), e0217670. doi:10.1371/journal.pone.0217670
人工智能支持的抛物线反应面平台可识别由已获批药物组成的超快速近乎通用的结核病药物治疗方案。Artificial intelligence enabled parabolic response surface platform identifies ultra-rapid near-universal TB drug treatment regimens comprising approved drugs. PLOS ONE, 14(5), e0217670. doi:10.1371/journal.pone.0217670
该研究的作者,戴维·格芬医学院的医学和微生物学、免疫学和分子遗传学教授Marcus Horwitz博士表示,如果该研究结果在人体研究中得到重复,则患者将更快地治愈,更可能坚持药物治疗,药物毒性降低,并不太可能产生耐药结核病。
由于耐多药结核病和广泛耐药结核比普通(药物敏感性)结核的治疗时间要长出很多,且需要使用二线抗结核药物。后者更加昂贵,且与治疗药物敏感性结核所用的一线药物相比具有更多副作用。因此,对于耐药性肺结核患者,早期诊断早期治疗很重要,但同样至关重要的是,利用能提供准确的方法,以便在尽可能短的时间内结束治疗,使患者最大受益。期待未来通过科研人员的探索和实践,使这些新药与新技术尽快落地,减轻患者的负担。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#耐药性肺结核#
82
棒棒棒
120
非常棒的文章,鼓掌
113
#新突破#
69
#结核#
65
评论
121