EAU18∣魏强教授团队:区域淋巴结及远处转移性前列腺癌的局部治疗研究进展
2018-03-24 廖鑫扬 魏强 肿瘤瞭望
前列腺癌是威胁男性健康的常见肿瘤之一,全世界发生率位列男性肿瘤的第2位。初诊转移性前列腺癌患者5年生存率仅为28%。内分泌治疗及化疗是转移性前列腺癌的标准治疗方案,虽然能提高转移性前列腺癌患者的短期生存率,但对患者的远期生存率影响不大,且并发症较多。
前列腺癌是威胁男性健康的常见肿瘤之一,全世界发生率位列男性肿瘤的第2位。初诊转移性前列腺癌患者5年生存率仅为28%。内分泌治疗及化疗是转移性前列腺癌的标准治疗方案,虽然能提高转移性前列腺癌患者的短期生存率,但对患者的远期生存率影响不大,且并发症较多。
2014年StephenCulp基于美国SEER(癌症监测、流行病学和结果数据库)进行的研究显示局部治疗(手术治疗及内照射放疗)可使转移性前列腺癌患者获益,转移性前列腺癌的局部治疗自此备受关注。如何在精准医学的大背景下,为转移性前列腺癌患者选择合适治疗方案,提高生存时间,降低肿瘤特异性死亡率,仍是越来越多临床研究尝试去探索和解决的问题。
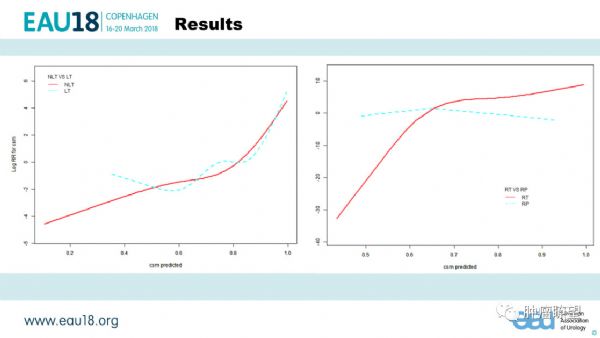
在本次会议上,四川大学华西医院魏强教授团队在上述研究的基础上更进一步,提出了针对肿瘤原发灶局部治疗(根治性手术或放疗)适用人群的方案决策模型。为减少观察偏倚,研究利用既往病历资料分析,纳入了2004年-2014年的12780名转移性前列腺癌患者(235人接受了前列腺癌根治手术、237接受了前列腺内照射放疗,12251人未接受局部治疗)。为控制选择偏倚,在1:4的倾向评分匹配后,收集可能与疗效有关的基线资料(年龄、性别、种族、肿瘤转移负荷、肿瘤体积、PSA、肿瘤分级等)。
研究使用广义相加混合模型建立死亡的预测模型(用基线资料预测患者5年内的死亡)。通过曲线拟合局部加权及交互作用检验,找到“适应症”:①预测死亡风险<50%的患者,局部治疗比非局部治疗效果好,预测死亡风险≥50%的患者两种治疗方式效果差异不显着。②预测死亡风险<65%的患者,根治性手术的疗效更好;当预测死亡风险≥65%,放疗效果更好。该决策模型的临床意义及创新性受到了与会专家的一致认可,并提出了申请外部验证及考虑时间分段效应进一步优化模型等建设性意见。
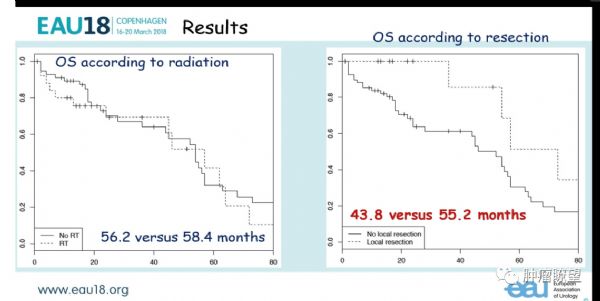
德国的Pompe教授团则利用SEER数据库,进一步探讨了基线PSA、前列腺癌M分期亚型与转移性前列腺癌局部治疗患者生存获益的关系。研究纳入了2004年-2014年的13906名转移性前列腺癌患者。结果发现两种局部治疗组肿瘤特异性死亡率均低于未接受局部治疗组。而治疗方式、基线PSA水平之间的交互关系,仅存在于M1b期中;在该亚型中,仅当患者基线PSA小于60ng/mL时,局部治疗可带给患者显着的生存获益。对于M1c期患者,局部治疗不能带来生存获益。对于M1a期患者,局部治疗带来显着生存获益,但与基线PSA的关系因样本量过小,尚缺乏证据。关于是否对转移性前列腺癌患者进行局部治疗,Pompe创新性地提出同时结合基线PSA水平与转移分期亚型进行考察,可谓令人眼前一亮。
今年EAU大会的另一项来自德国Heidenreich教授团队的研究提出,针对转移灶局部治疗能改善已经行减瘤性前列腺癌根治术的寡转移性前列腺癌患者的无恶化生存期和总体生存时间。该研究是目前样本量最大的接受减瘤手术的转移性前列腺癌患者的临床研究,也为转移性前列腺癌的治疗提供了新的视角。
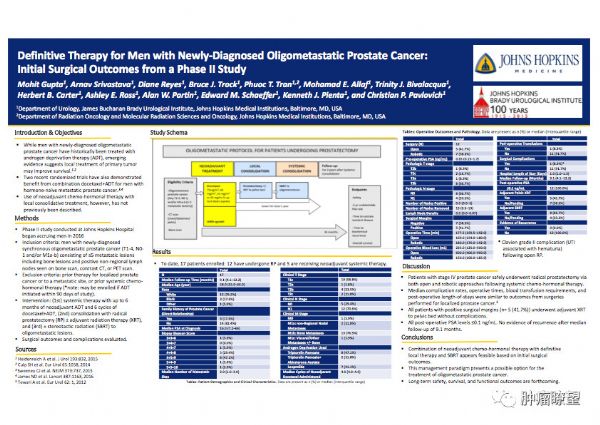
来自约翰霍普金斯大学的Gupta教授团队在本次大会上分享了其团队前列腺癌寡转移患者综合治疗二期试验的病人的手术情况。在该项研究中,前列腺癌寡转移患者共经历三阶段治疗:1)6个月的内分泌治疗和6周期的多西他赛化疗,2)前列腺癌根治术±术后放疗,3)转移灶的立体定位放疗。目前招募的24位受试者中已有12名进行过手术,术后PSA平均为0.4ng/mL,结合手术时间、术中失血、住院天数,现8名患者PSA已下降至不可检测水平。也许将来有望成为前列腺癌寡转移患者的标准治疗,不过长期的安全性、生存时间和功能学指标结局还有待检验。
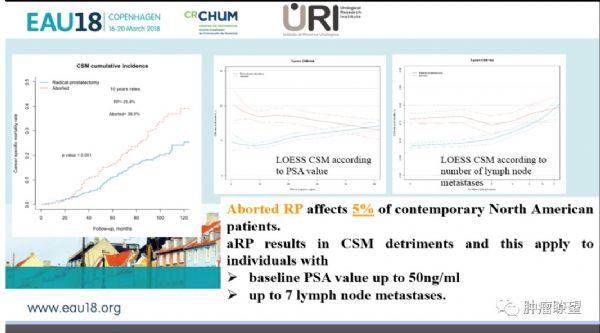
来自意大利米兰的Marco Bandini在本次EAU中展示的回顾性队列研究中,选取了2004年-2014年的拟行前列腺癌根治术且盆腔淋巴结清扫阳性的3761名患者,冰冻切片显示盆腔淋巴结有转移而放弃根治术的患者从2004的占比由2004年20.2%下降至2014年的5.6%,竞争风险存活分析显示,区域淋巴结转移性前列腺癌患者放弃根治术组10年肿瘤特异性死亡率显着高于完成根治术组,提示前列腺癌根治术带给区域淋巴结转移性前列腺癌患者的生存获益。
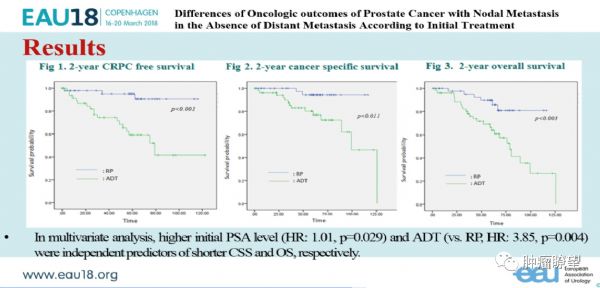
今年EAU大会中来自韩国的该项淋巴结转移性前列腺癌患者的回顾性研究中,纳入155例接受内分泌治疗的cN1淋巴结转移性前列腺癌患者、371例接受根治手术的pN1淋巴结转移性患者,发现接受内分泌治疗的淋巴结转移性患者总体生存时间明显低于根治手术组,提示淋巴结转移前列腺癌患者中,初始治疗采用根治手术的优越性。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EAU#
85
#淋巴结#
65
#研究进展#
57
#转移性#
96
#转移性前列腺癌#
81
#局部#
86
#远处转移#
95
#局部治疗#
56