JACC:连续高NSE值对OHCA不良结局有较强的预测性
2015-05-22 张旭栋译 MedSci原创
卢森堡中心医院Pascal Stammet博士等人探索了神经元特异性烯醇化酶对于院外心脏骤停不良结局的预测性,并同时探索了温度管理对其的影响,研究成果发表在5月份的Circulation期刊上。背景: 神经元特异性烯醇化酶(NSE)是心脏骤停后神经系统预后的一种广泛使用的生物标志物,但是,由于缺乏标准化的方法和不确定的温度管理影响,推荐的临界值相关性一直备受质疑。目的: 本研究旨在
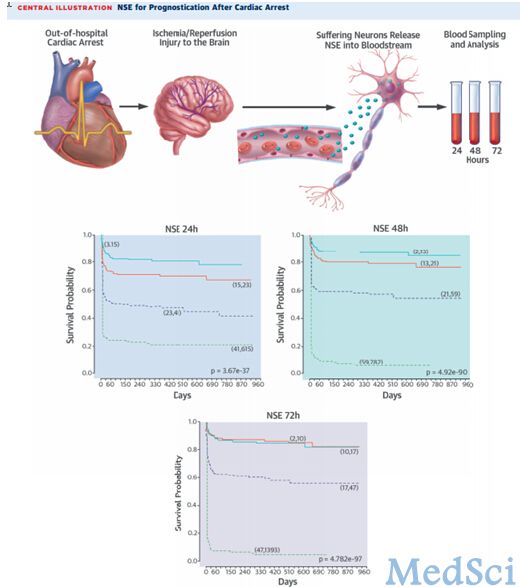
卢森堡中心医院Pascal Stammet博士等人探索了神经元特异性烯醇化酶对于院外心脏骤停不良结局的预测性,并同时探索了温度管理对其的影响,研究成果发表在5月份的Circulation期刊上。
背景:
神经元特异性烯醇化酶(NSE)是心脏骤停后神经系统预后的一种广泛使用的生物标志物,但是,由于缺乏标准化的方法和不确定的温度管理影响,推荐的临界值相关性一直备受质疑。
目的:
本研究旨在探索院外心脏骤停(OHCA)患者中NSE对于预后起到的预测作用。
研究纳入了686例OHCA住院患者,将其随机分配为33℃或36℃温度管理组。自主循环恢复分别为24,48,72小时后评估血液样品中NSE的水平值。主要结局是6个月后,通过神经功能CPC评分(cerebral performance category score)从而评价神经系统结局。
结果:NSE对于神经系统结局有着显著的预测性,目标温度不会显著影响NSE值。24,48,72小时候,有利结局与不利结局中位NSE比值分别为18ng/ml比35ng/ml,15ng/ml比61ng/ml,以及12ng/ml比54ng/ml(P<0.001)。48和72小时,NSE通过ROC曲线下的面积从而对于神经系统结局的预测值分别为0.85和0.86。高NSE值的假阳性率≤5%,95%置信区间能够可靠地预测结果。
结局:
连续高NSE值对OHCA不良结局有较强的预测性。33℃或36℃温度管理对于NSE水平并没有显著的影响。
原始出处:
Stammet P, Collignon O, Hassager C, et al. Neuron-Specific Enolase as a Predictor of Death or Poor Neurological Outcome After Out-of-Hospital Cardiac Arrest and Targeted Temperature Management at 33 degrees C and 36 degrees C. Journal of the American College of Cardiology. 2015;65(19):2104-14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#HCA#
61
#JACC#
60
看看
165
#ACC#
95