Ann Oncol:紫杉醇联合或不联合atezolizumab一线治疗不可切除、局部晚期或转移性三阴性乳腺癌的疗效: IMpassion131初次分析
2021-07-04 yd2015 MedSci原创
atezolizumab联合紫杉醇对比紫杉醇单药并不能改善不可切除、局部晚期或转移性三阴性乳腺癌(TNBC)患者的PFS或OS。
免疫治疗在晚期三阴性乳腺癌(TNBC)中展示出一定疗效。比如III期临床研究IMpassion130,主要评估 atezolizumab联合白蛋白结合型紫杉醇(A + nP)对比安慰剂联合白蛋白结合型紫杉醇(P+nP)一线治疗既往未治疗的,不可切除、局部晚期或转移性TNBC的疗效和安全性。结果表明,对于肿瘤浸润免疫细胞(IC)PD-L1阳性TNBC患者,(A + nP)组较(P+nP)组明显改善患者的OS。III期临床研究KEYNOTE-355表明pembrolizumab联合化疗可改善TNBC的PFS。因此,有研究者开展IMpassion131研究,评估紫杉醇联合或不联合atezolizumab一线治疗不可切除、局部晚期或转移性三阴性乳腺癌的疗效,结果发表在Annals of Oncology杂志上。
IMpassion131是全球,随机,双盲,安慰剂对照III期试验。主要研究终点是研究者评估的PFS。次要研究终点是OS和客观缓解率(ORR)。2017年8月25日至2019年9月5日,来自欧洲、北美和南美、亚洲和非洲的150研究中心的651名患者被纳入研究; 431名患者随机接受atezolizumab联合紫杉醇治疗,220名患者随机接受安慰剂联合紫杉醇治疗。651例患者中有292例(45%)为PD-L1阳性(IC ≥1%)。
截止2019年11月15日,进行首次PFS分析。PD-L1阳性患者中,atezolizumab联合紫杉醇组和安慰剂联合紫杉醇组的中位随访时间分别为9个月和8.6个月。ITT人群中,两组的中位随访时间分别为8.8个月和8.5个月。PD-L1阳性人群中,atezolizumab的加入并不能改善患者的PFS,两组的中位PFS分别为6.0个月和5.7个月 (HR=0.82, 95% CI 0.60-1.12; log-rank P=0.20)。在ITT人群中,两组的中位PFS分别为5.7个月和5.6个月(HR=0.86, 95% CI 0.70-1.05))。敏感性分析,独立审查委员会评估的PD-L1阳性人群PFS的HR= 0.73 (95% CI 0.54-1.00)。
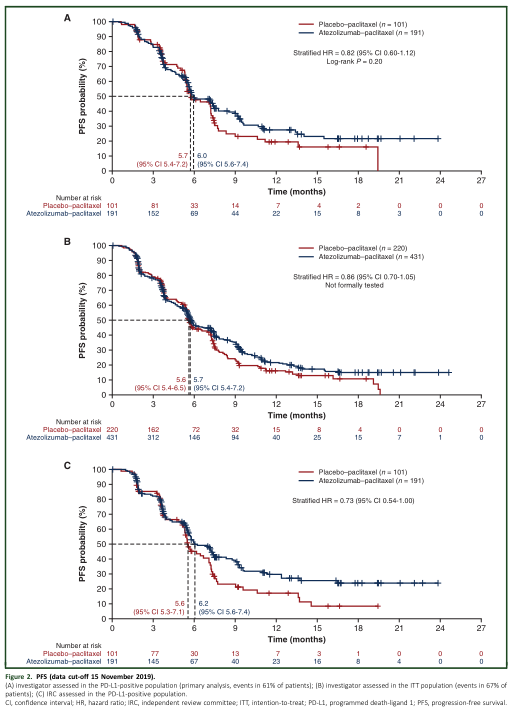
PFS
截止2020年9月4日最终OS分析,PD-L1阳性患者中,atezolizumab联合紫杉醇组和安慰剂联合紫杉醇组的中位随访时间分别为15.2个月和15.8个月。ITT人群中,两组的中位随访时间分别为14.2个月和14.5个月。PD-L1阳性人群中,两组的中位OS分别为22.1个月和28.3个月 (HR=01.11, 95% CI 0.76-1.64)。1年的OS率分别为75% (95% CI 68-81%)和83%(95% CI 76-91%);2年OS率分别为48% (95% CI 39-57%)和51% (95% CI 37-64%)。在ITT人群中,两组的中位OS分别为19.2个月和22.8个月(HR=1.12, 95% CI 0.88-1.43))。1年的OS率分别为69% (95% CI 64-73%)和73% (95% CI 67-79%);2年OS率分别为42% (95% CI 36-48%) 和 45% (95% CI 36-54%)。

OS
两组严重的不良事件(AEs)发生率分别为25%和18%;3/4 级AEs分别为53%和46%;5 级AEs 均为2%。最常见的AEs (每组均≥25%)为为脱发、贫血、周围神经病变、腹泻、疲劳和恶心。
综上,atezolizumab联合紫杉醇对比紫杉醇单药并不能改善不可切除、局部晚期或转移性三阴性乳腺癌(TNBC)患者的PFS或OS。
原始出处:
D. Miles, J. Gligorov, F. André, et al. Primary results from IMpassion131, a double-blind, placebo-controlled, randomised phase III trial of first-line paclitaxel with or without atezolizumab for unresectable locally advanced/metastatic triple-negative breast cancer. Annals of Oncology, 2021, https://doi.org/10.1016/j.annonc.2021.05.801.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SSI#
63
#转移性三阴性乳腺癌#
0
#mAb#
49
#Oncol#
62
#局部晚期#
47
#阴性乳腺癌#
48
#转移性#
55
#局部#
0
#三阴性#
56
谢谢梅斯提供这么好的信息,学到很多
0