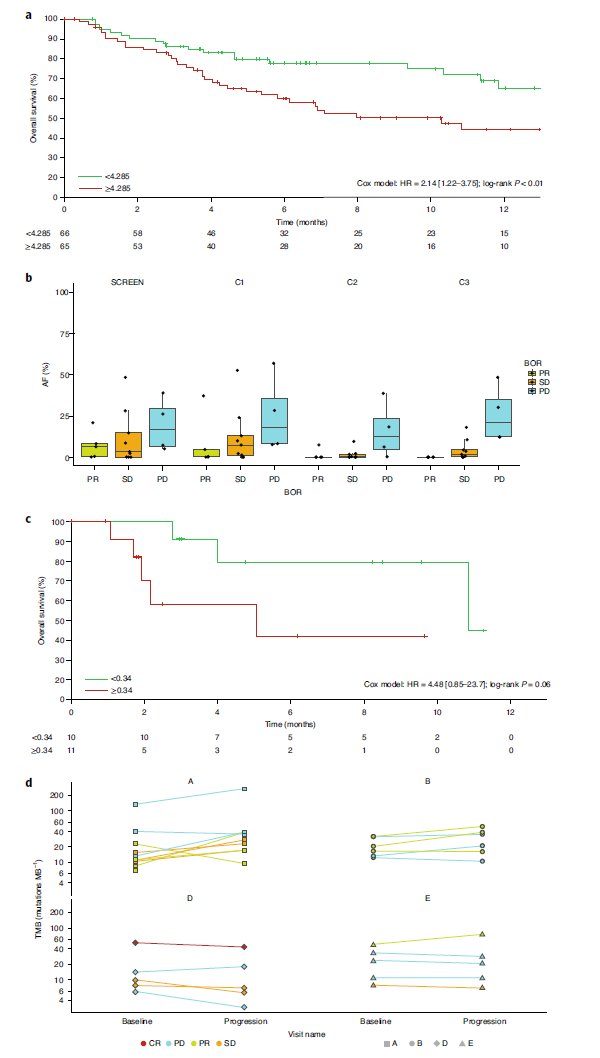
Nat Med:Durvalumab联合靶向疗法治疗晚期尿路上皮癌
2021-05-05 xiaozeng MedSci原创
基于铂的化学疗法目前仍是尿路上皮癌(AUC)的最广泛使用的全身疗法。
基于铂的化学疗法目前仍是尿路上皮癌(AUC)的最广泛使用的全身疗法。而免疫检查点抑制剂(例如PD-L1抑制剂)作为标准疗法,从理论上而言,靶向/免疫疗法的联合治疗可以提高患者的缓解率(RR)并更好地维持反应的持久性。
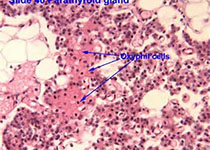
德瓦鲁单抗(Durvalumab)是一种PD-L1(编程性死亡配体1)抑制剂,研究人员发现其在晚期AUC中具有临床活性。AUC的特征表现为几个可反复靶向的基因组改变。
该研究旨在测试durvalumab与AUC中三种靶向药物之一联合使用的安全性,并分析其是否可以提高药物的临床活性。
这项研究(NCT02546661,BISCAY)通过在生物标志物选择的化疗难治性AUC人群中将durvalumab与相关靶向治疗相结合,主要与以上三种药物联用:(1)对具有FGFR DNA突变(FGFRm)肿瘤联用FGFR(成纤维细胞生长因子受体)抑制剂;(2)对具有和没有DNA同源重组修复缺陷(HRRm)肿瘤联用PARP(多聚ADP核糖聚合酶)药理抑制剂;(3)对具有mTOR/PI3K通路DNA突变肿瘤联用TORC1/2抑制剂。
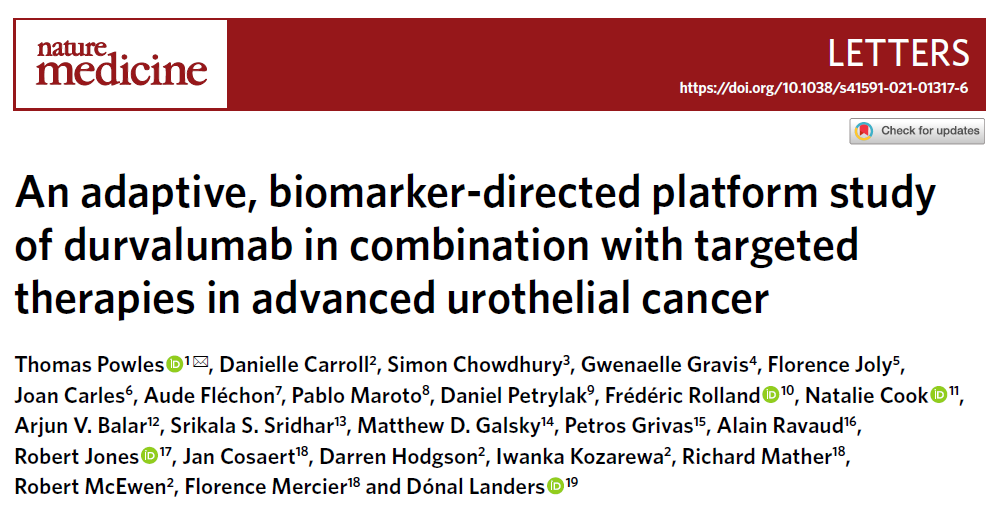
BISCAY研究不同组的疗效数据
该试验采用了一种新型的、由生物标记物驱动的多臂适应性设计,主要评估药物的安全性、功效和相关的生物标志物。研究人员共收集了391例患者,其中筛选的135例患者被分配到六个研究组别中。
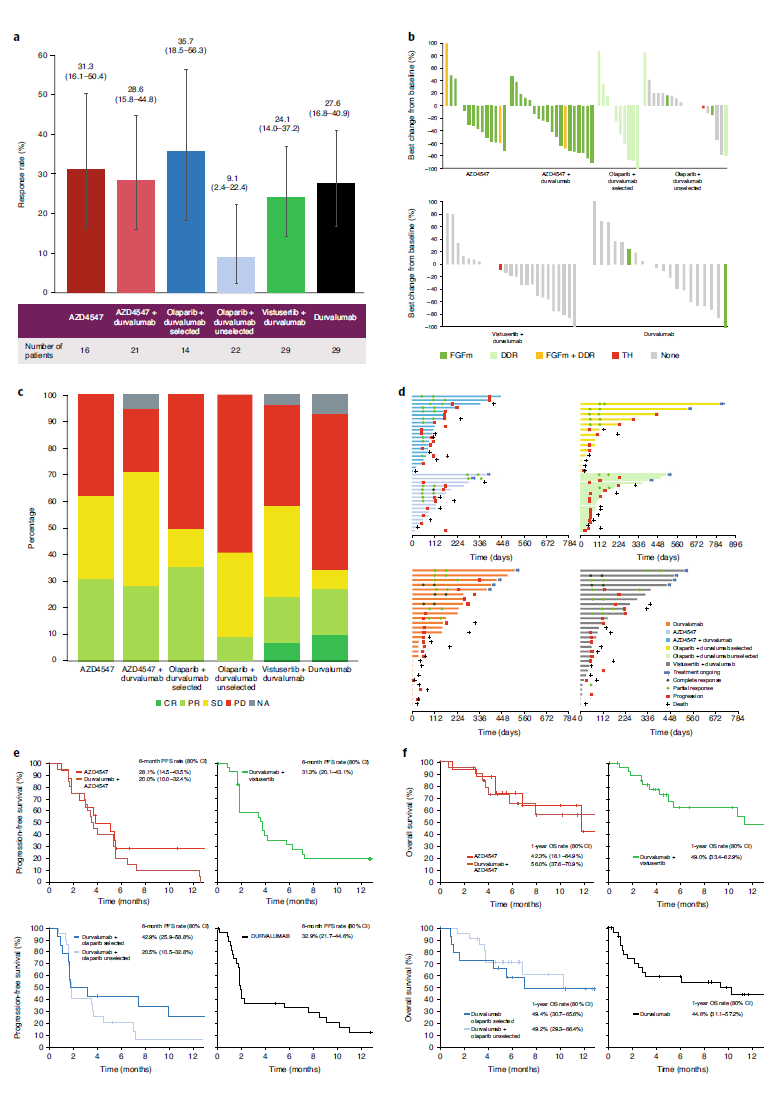
结果显示,研究组的缓解率(RRs)为9–36%,并不符合进一步开发的疗效标准。联合治疗组和durvalumab单药治疗组患者的总生存期(OS)和无进展生存期(PFS)相似。生物标志物分析显示出了ctDNA(循环肿瘤DNA)与FGFRm组织之间的相关性。ctDNA分析结果也表明,FGFRm的变化与临床结果相关。
FGFR突变ctDNA与治疗应答的相关性
总而言之,该研究结果支持了FGFR抑制剂和durvalumab单药治疗的临床活性,但未证实联合治疗药物活性的增加。这些发现也为AUC中的靶向/免疫治疗方法提出了一定的疑问,还有待进一步的研究确认。
原始出处:
Powles, T., Carroll, D., Chowdhury, S. et al. An adaptive, biomarker-directed platform study of durvalumab in combination with targeted therapies in advanced urothelial cancer. Nat Med (03 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
50
#联合靶向#
39
#mAb#
28
#靶向疗法#
42
#晚期尿路上皮癌#
54
#上皮癌#
33
#Med#
33