BMC Gastroenterol:Graves病与慢性乙型肝炎、甲巯咪唑所致肝损伤及自身免疫性肝炎重叠1例
2022-03-04 从医路漫漫 MedSci原创
与甲状腺机能亢进症相关的肝功能障碍包括甲状腺激素过多、药物性肝损伤和伴随肝病引起的改变。

背景:与甲状腺机能亢进症相关的肝功能障碍包括甲状腺激素过多、药物性肝损伤和伴随肝病引起的改变。他巴唑(MMI)是临床上用于治疗Graves病(GD)的一线抗甲状腺药物,Graves病是最常见的甲状腺机能亢进症(甲亢)的病因。MMI也与一定程度的肝损伤有关,尽管其副作用没有丙基硫氧嘧啶(PTU)严重。临床上,MMI引起的肝毒性的特征是多种多样的,包括坏死性炎症、肉芽肿和/或脂肪变性,主要表现为胆汁淤积。与Graves病(GD)相关的肝损伤包括甲状腺激素过多引起的肝毒性、药物性肝损伤以及伴发肝病引起的改变。他巴唑(MMI)可引起多种形式的肝损伤。然而,自身免疫性肝炎(AIH)与GD或慢性乙型肝炎重叠的诊断和治疗是具有挑战性的。
病例介绍:一位来自中国的35岁男性患者,有两年的GD病史和10天的进行性黄疸病史。一年前,他服用了两个月的MMI,由于肝脏毒性而停止治疗,并在住院前20天又服用了6天。患者入院时被诊断为GD重叠慢性乙型肝炎和MMI所致肝损伤,并伴有早期急性-慢性肝功能衰竭。但在纠正肝功能衰竭、有效控制HBV复制和甲亢后,每日口服恩替卡韦和一次性口服131I均不能控制升高的转氨酶和胆红素水平。患者于入院第43天行肝活检,肝细胞膜表面有HBsAg表达,具有典型的AIH组织病理学特征。他最终被诊断为GD重叠慢性乙型肝炎、MMI诱导的肝损伤和AIH。经3个月糖皮质激素治疗和持续恩替卡韦治疗后,升高的转氨酶和胆红素完全恢复正常,随访6个月未见复发,提示该患者的AIH不同于经典的AIH或GD相关的AIH。
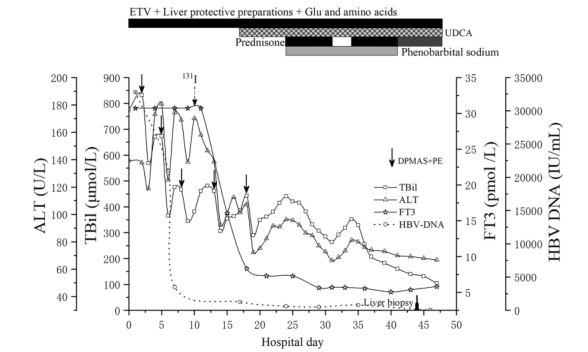
图1住院期间实验室检查结果。丙氨酸氨基转移酶,总胆红素,游离三碘甲状腺原氨酸,乙型肝炎病毒脱氧核糖核酸,ETV恩替卡韦,熊去氧胆酸,葡萄糖,DPMAS双血浆分子吸附系统,PE,血浆交换
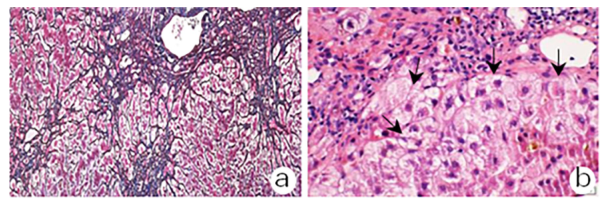
图2 住院期间实验室检查结果。Masson三色和网状纤维染色显示部分相邻的汇管区相连,分隔周围肝实质和轻度间质纤维化;b HE染色显示汇管区有中度淋巴浆细胞浸润,明显的肝炎和肝细胞花环(箭头),肝细胞内胆色素颗粒和胆汁毛细血管内形成胆小管内的胆栓性病变;b HE染色显示汇管区有中度淋巴浆细胞浸润,肝细胞内有明显的交界性肝炎和肝细胞花环(箭头),肝细胞内有胆色素颗粒,毛细血管内有胆栓形成。
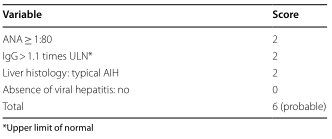
表1使用简化评分系统的自身免疫性肝炎评分

表2 GD与AIH的区别
结论:GD合并AIH是一个复杂而困难的课题。需要澄清的是,MMI或HBV是否可以作为该患者AIH的触发因素。
原文出处:Zheng M, Cui S, Zhang W,et al.Graves' disease overlapping with chronic hepatitis B and methimazole-induced liver injury and autoimmune hepatitis: a case report.BMC Gastroenterol 2022 Feb 10;22(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#乙型肝炎#
85
#Gastroenterol#
51
#AST#
46
#GAS#
53
#Graves#
78
#BMC#
48
少见病也不少见
100
受益匪浅
93
学习了
96
#慢性乙型肝炎#
78