RADIOLOGY:后颅窝减压术后Chiari畸形小脑和脑干位移明显减少
2021-07-30 MedSci原创 MedSci原创
后颅窝减压术后神经组织位移减少,表明手术干预改变了脑组织生物力学。对于Chiari畸形I型的受试者,没有发现术前组织移位与术前症状之间的关系。

Chiari畸形I型(CMI)定义为小脑扁桃体下降至枕骨大孔至少5毫米以下。CMI患者存在多种神经症状,包括枕下头痛和/或颈部疼痛、认知和/或神经功能缺损以及一系列非特异性症状。CMI患者可接受后颅窝减压(PFD)手术,以减轻症状,恢复后颅窝脑脊液流动,减少扁桃体拥挤,减轻脑干和/或小脑组织压迫。尽管术前评估包括扁桃体下降和其他形态学特征的评估,但关于扁桃体下降是否与CMI症状相关的文献中存在相互矛盾的结果。后颅窝减压术(PFD)是治疗Chiari畸形I型(CMI)的一种方法。手术的目的是减少小脑扁桃体拥挤和恢复后部脑脊液流动,但局部组织生物力学也可能发生变化。基于MRI的受激回波位移编码(DENSE)可用于神经组织位移的评估。
Maggie S. Eppelheimer等应用MRI技术评价CMI患者PFD手术前后的神经组织移位情况,并探讨组织移位与症状之间的关系。

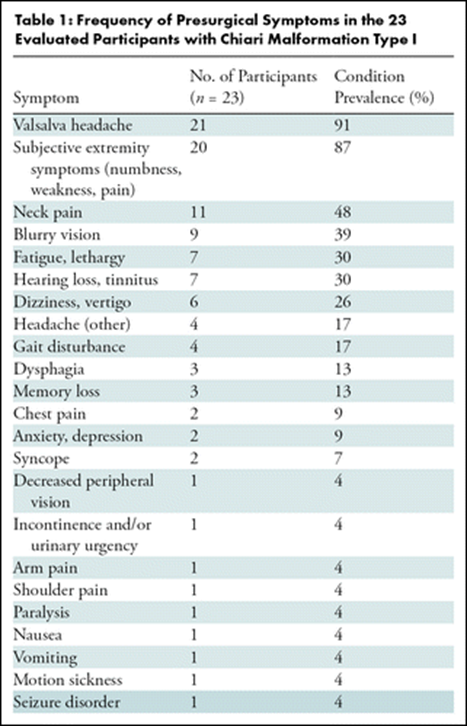
对CMI患者进行前瞻性HIPAA依从性研究,于2017年1月至2020年6月间在PFD手术前后进行中矢状面MRI检查。在心动周期内,小脑和脑干组织位移峰值被量化,每个结构的平均值,并在手术前和手术后进行比较。使用配对t检验和非参数Wilcoxon符号秩检验来确定移位的手术改变,并确定组织移位和预诊症状之间的Spearman相关性。
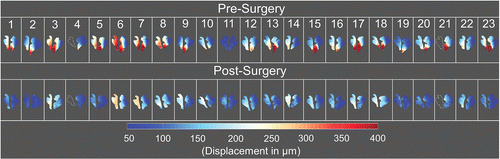
所有参与者手术前后脑干和小脑的峰值位移图。
23名受试者(平均年龄±标准差,37岁±10岁;19名女性)。术后小脑内的空间平均峰值组织位移减少了46%(79/171μm),脑干内减少了22%(46/210μm)(P<.001)。在30 mm2圆形区域内计算的最大峰值位移,小脑减少64%(274/427μm),脑干减少33%(100/300μm)(P<.001)。组织移位与CMI症状之间无显著相关性(r<.74,P>.012;Bonferroni校正P=.0002)。
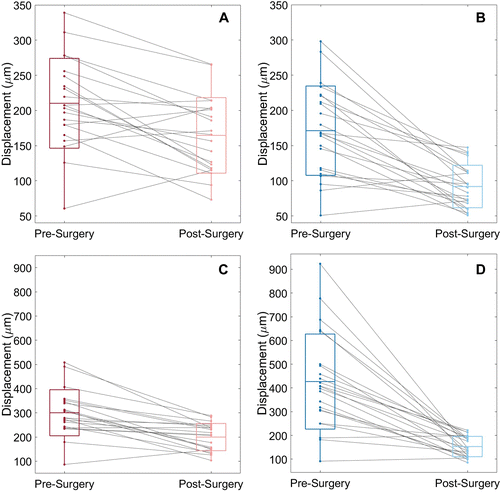
23名受试者在手术前和手术后(A,C)脑干和(B,D)小脑的平均和最大峰值位移
通过使用基于MRI的受激回声位移编码发现后颅窝减压术(PFD)后小脑和脑干位移减少,手术对小脑运动的影响比对脑干运动的影响更大。结果表明,PFD手术不仅改变了解剖结构,而且改变了潜在的脑组织运动和生物力学,在空间上是不均匀的。虽然发现手术后小脑和脑干运动减少,但这种减少不能预测术前Chiari畸形I型(CMI)症状。
总之,后颅窝减压术后神经组织位移减少,表明手术干预改变了脑组织生物力学。对于Chiari畸形I型的受试者,没有发现术前组织移位与术前症状之间的关系。此外,尽管移位与CMI症状无关,但其他脑生物力学特性,如劳损,可能是CMI症状的预测因素。
原文出处
Cerebellar and Brainstem Displacement Measured with DENSE MRI in Chiari Malformation Following Posterior Fossa Decompression Surger
https://pubs.rsna.org/doi/10.1148/radiol.2021203036
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Chiari畸形#
74
#畸形#
93
hao
88
好
90
很棒
85