Heartwire:ICD手术期间应用华法林或优于肝素过渡
2013-05-15 高晓方 译 医学论坛网
第34届美国心律学会年会(HRS 2013)公布的BRUISE CONTROL研究表明,在起搏器或置入型心律转复除颤器(ICD)手术期间,继续应用华法林可能较肝素过渡更为适宜。研究同时在线发表于2013年5月9日的《新英格兰医学杂志》(NEJM)上。 此项研究共纳入681例需行起搏器或ICD手术的患者,338例在术前接受肝素过渡治疗,343例继续接受华法林治疗。结果显
第34届美国心律学会年会(HRS 2013)公布的BRUISE CONTROL研究表明,在起搏器或置入型心律转复除颤器(ICD)手术期间,继续应用华法林可能较肝素过渡更为适宜。研究同时在线发表于2013年5月9日的《新英格兰医学杂志》(NEJM)上。
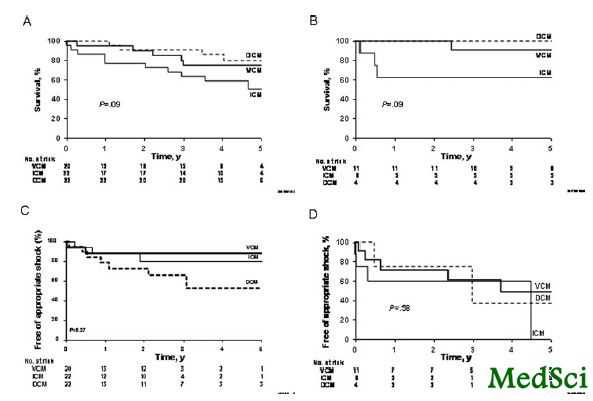
此项研究共纳入681例需行起搏器或ICD手术的患者,338例在术前接受肝素过渡治疗,343例继续接受华法林治疗。结果显示,肝素过渡组的临床相关性装置血肿的发生率显著高于华法林组(16%对3.5%;P<0.001)。严重手术和血栓形成并发症稀少,并且两组之间无差异。华法林组患者的中位INR2.3与围手术期大出血无关,但与患者满意度升高相关。
与华法林相关的拓展阅读:
- Circulation:阿派沙班在不同治疗时间窗内均优于华法林
- NEJM述评:达比加群引起的出血风险不高于华法林
- PACE:房颤射频消融围手术期患者使用达比加群优于华法林
- JAMA:生物主动脉瓣植入后六个月行华法林治疗应设为标准
- NEJM:华法林与阿司匹林在心脏射血分数降低患者中的疗效比较 更多信息请点击:有关华法林更多资讯
BRUISE CONTROL: Continued warfarin beats heparin bridging in ICD/pacemaker implants
Patients at high risk of thromboembolism who require pacemaker or implantable cardioverter-defibrillator (ICD) surgery can safely remain on warfarin, without interruption, rather than be bridged with heparin, results of the BRUISE CONTROL study suggest [1].
Dr David H Birnie (Ottawa Heart Institute, ON) and colleagues report their findings online May 9, 2013 in the New England Journal of Medicine, timed to coincide with Birnie's presentation of the study at the Heart Rhythm Society (HRS) 2013 Scientific Sessions.
Guidelines currently recommend that patients at high risk for thromboembolic events be bridged with heparin therapy, with their warfarin stopped five days before their procedure, the group notes. But few randomized, controlled studies have actually given the strategy a proper test, especially compared with simply maintaining patients on warfarin throughout their procedures.
In BRUISE CONTROL's >600 patients who at baseline had a predicted annual stroke risk of >5%, the continued-warfarin approach was associated with a "highly significant reduction in the rate of device-pocket hematoma compared with heparin bridging," Birnie noted when formally presenting the trial at the HRS sessions. The risk of that primary end point was reduced by 81% (p<0.001).
"We also found that operating with continued warfarin, with a median [international normalized ratio] INR of 2.3, was not associated with any major perioperative bleeding events," he said.
At a press conference on the trial, Birnie observed that all the components of the primary end point, which reflected different kinds of pocket hematoma, were significantly reduced in the continued-warfarin group. "So the study was unequivocally positive."
Reporters asked Birnie whether the trial's findings in patients who took warfarin or, if bridged, low-molecular-weight heparin or unfractionated heparin, could be extrapolated to surgery-scheduled patients who are on dabigatran (Pradaxa, Boehringer Ingelheim), rivaroxaban (Xarelto, Bayer/Johnson & Johnson), or apixaban (Eliquis, Bristol-Myers Squibb/Pfizer).
"This does not in any way apply to the new agents," he said. "The whole risk/benefit ratio with the new agents is completely different from [that of] warfarin. Their onset of action is in hours as opposed to five days."
The trial had randomized 338 patients to heparin bridging and 343 to warfarin continuation by the time the data safety monitoring board recommended early termination. A second prespecified interim analysis suggested a significant advantage for warfarin continuation. The rate of clinically relevant pocket hematoma was 16% in the heparin-bridging group and only 3.5% in the continued-warfarin group (p<0.001).
Relative risk (RR) for outcomes, continued warfarin (n=343) vs heparin bridging (n=338)

Major surgical and thrombotic complications were few, with no significant differences between treatment groups.
Moreover, Birnie observed in his presentation, "patients in the continued- warfarin arm had much greater satisfaction with their perioperative anticoagulation management." That was reflected in their higher scores on the seven-point Likert scale, which averaged 6.4 in contrast to 5.9 for patients in the heparin-bridging group (p<0.001).
After Birnie's presentation, session comoderator Dr John D Day (Intermountain Medical Center, Salt Lake City, UT) asked him whether the trial has influenced practice at his center. He also asked what other influences on outcomes were observed.
"For sure, our clinical practice changed as soon as we saw these results," Birnie replied. And "there were only three independent predictors of pocket-hematoma formation in multivariate analysis. Number one, and far and away the most important, was to do it on continued warfarin. Number two, aspirin doubled the risk of pocket hematoma. Number three, a result that was a surprise to us: the presence of diabetes seemed to be protective against pocket hematoma."
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#手术期#
63
#ICD#
51
#ART#
31
#HEART#
46