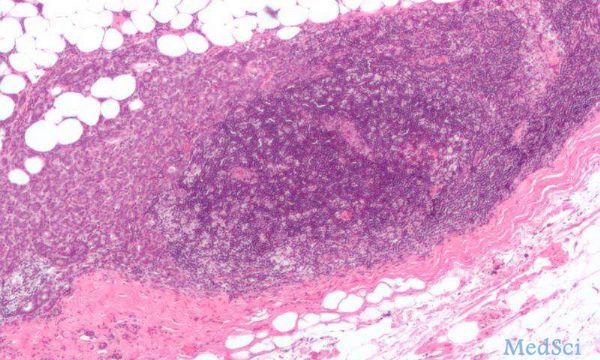
SCI REP:多巴胺D1受体激动剂可以抑制乳腺肿瘤及骨转移进展
2017-04-05 MedSci MedSci原创
在中枢神经系统中,多巴胺能信号通路扮演者重要的角色。多巴胺能信号通路参与调节认知、记忆、学习等多项功能。其功能异常与帕金森病、精神分裂症等发病息息相关。已知的多巴胺受体有D1-D5,可以分为D1类受体以及D2类受体。激动D1类受体可以诱导腺苷酸环化酶,增加细胞内cAMP水平。乳腺癌死亡首要原因并不是原发肿瘤,而是后续的肿瘤转移。其中骨转移是常见的转移方式。目前对于多巴胺能信号通路在乳腺癌及骨转移中
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乳腺肿瘤#
90
#激动剂#
82
学习了谢谢分享
110
宣传册才吃饭滚滚滚
119
脱光光观后感
115