JAMA:脓毒症休克的新定义和临床评价标准
2016-02-23 zhaoshuang 译 MedSci原创
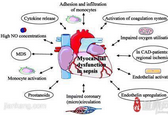
背景和目的:脓毒症休克是指一种与感染有关的急性循环衰竭的状态。新的生物学研究和流行病学挑战改变了其原本定义的有效性。本研究的目的是探讨成人脓毒症休克的新定义和临床标准。
Manu Shankar-Hari, MD, MSc,et al,Developing a New Definition and Assessing New Clinical Criteria for Septic Shock,For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3),JAMA. 2016;315(8):775-787. doi:10.1001/jama.2016.0289.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了.谢谢作者分享!
90
学习了.谢谢作者分享!
94
#新定义#
56
#脓毒症休克#
81
#临床评价#
70
不错,证据充分
157
不需要sirs和感染指标么
119
学习了 很不错
137
#评价#
50
#评价标准#
99