上海首例!伤口仅7mm,中山医院神外团队微创技术治疗头痛取得新突破
2022-03-15 复旦大学附属中山医院 网络
通过经皮穿刺全脊柱内镜下颈2神经节切除术,术后三个月,张阿婆的疼痛几乎消失了,不再服用任何止痛药物。
什 么 是 头 痛?
头痛是临床上非常常见的病症,病因不一,种类繁多,严重影响病患的生活质量,造成沉重的社会负担。颈部和后枕部的疼痛常常和上颈椎相关。其中,枕神经痛,又称颈2神经痛,来源自颈椎第2对神经。
按照国际头痛协会的定义,是指枕大神经、枕小神经以及第三对枕神经支配区域的疼痛,这种间歇性发作的疼痛呈枪击样、刀刺样,在头部活动时往往加重。而且,有时疼痛会不仅仅局限在枕部,会像头顶、颞部和眼眶周围扩散。患者往往脖子固定,难以活动,影响夜晚睡眠和日常生活,非常痛苦。
小萱和您说一个阿婆的案例
83岁的张阿婆近2年自觉左颈部刺痛放射至枕骨、头部、左颞部和眶周区域,只要有颈部活动就会加重疼痛,严重影响日常生活,这让她痛不欲生、夜不能寐。张阿婆去医院经历了保守治疗、3次神经阻滞治疗和2次脉冲射频(PRF)治疗后,也只能缓解50%的疼痛感,并且每次治疗后也仅能维持至多一个月的疼痛缓解,过了这个时限,“熟悉的疼痛感觉就又回来了!”
万般无奈下,张阿婆来到复旦大学附属中山医院神经外科余勇副主任医师诊室寻求帮助,经过完善的检查后,张阿婆被诊断为“顽固性枕神经痛”,在充分的术前评估以及与患者的沟通后,余医生团队决定为张阿婆行经皮穿刺全脊柱内镜下颈2神经节切除术。术后,患者疼痛明显减轻,仅有左枕部和颈后部稍麻木,症状轻微,对日常生活影响不大。该麻木也于1周后自行逐渐消失。术后三个月,张阿婆左枕部、颞部、眶上区、头顶和颈后部疼痛几乎消失了,不再服用任何止痛药物,并且这些区域也没有麻木。C1-2左侧椎旁压痛已不明显。前不久,又到了电话随访患者的日子,余医生按照惯例拨通了已随访2年多的张阿婆的电话,“真的太感谢余医生团队了,治好了困扰我多年的老毛病,手术后这些疼痛就真的消失了,太神奇了!”张阿婆在电话里激动地说。
近期,在复旦大学附属中山医院神经外科张晓彪主任的指导下,该科脊柱脊髓亚专业余勇副主任医师团队通过微创外科手术在治疗头痛领域取得突破,团队利用经皮穿刺脊柱内镜技术,成功治疗顽固性枕神经痛系列病例。该项具有原创性的手术方式在神经外科权威期刊《Operative Neurosurgery》(神经外科手术)上以封面文章形式发表,将对外科治疗头痛产生深远影响。
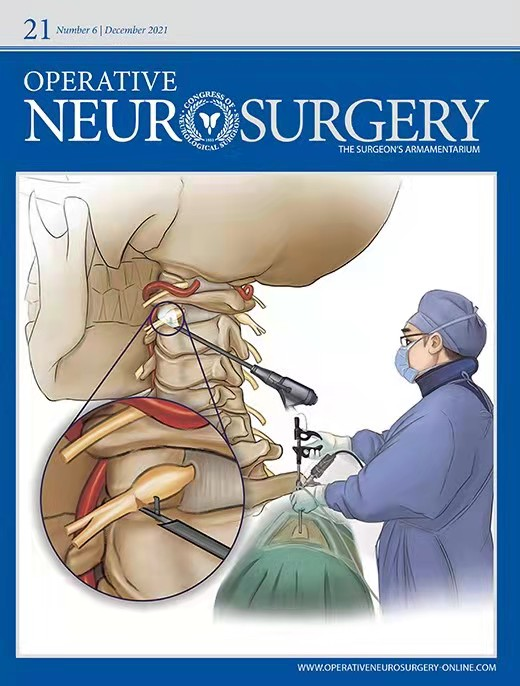
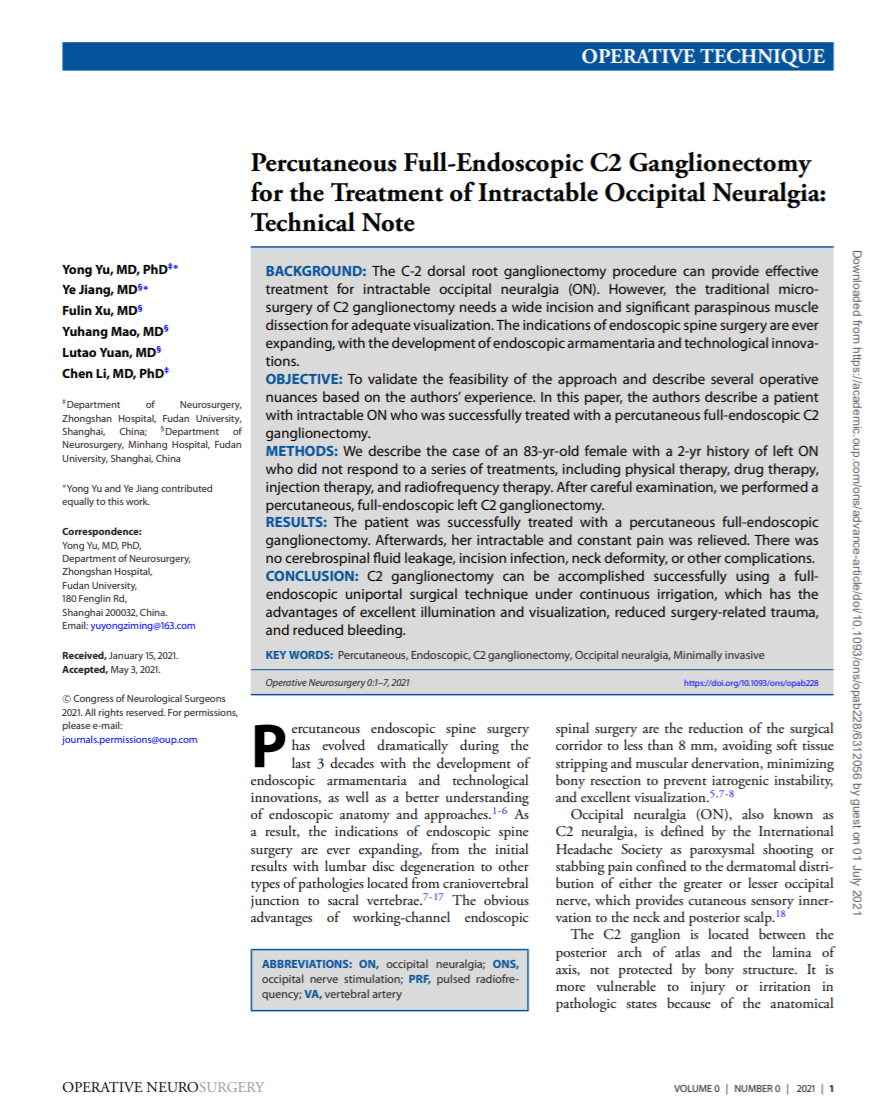
杂志封面和文章封面
上文提到的让张阿婆摆脱头痛的手术即是余勇副主任医师团队完成的上海首例利用经皮穿刺脊柱内镜技术成功治疗顽固性枕神经痛的病例。
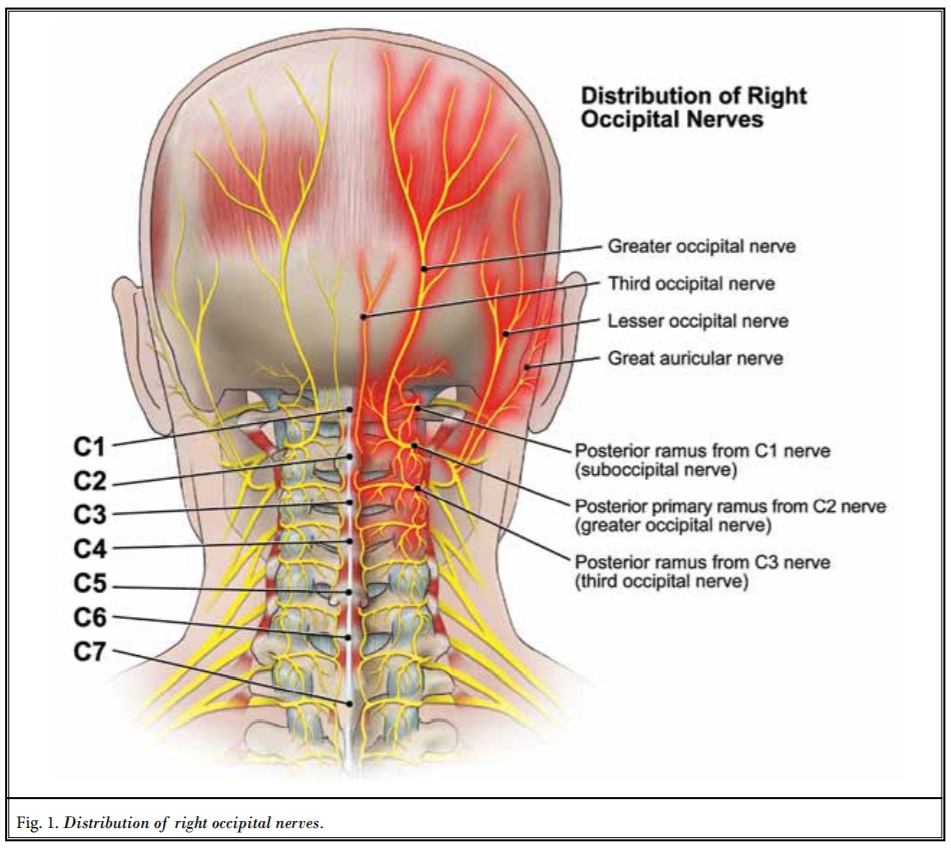
右侧枕神经疼痛模式图
枕神经痛的治疗原则应遵循阶梯治疗的方式,即首先是保守治疗,包括药物治疗、物理治疗等,再是神经阻滞、射频等介入治疗,介入治疗无效的顽固性枕神经痛患者可以考虑手术治疗。
既往的外科术式包括神经松解减压、神经根切断等治疗方法,但这些方式常因神经再生和神经瘤形成导致术后疼痛复发。枕神经刺激术(ONS)是近年来难治性枕神经痛的一种有潜力的治疗方法,其方法需在颈部植入电极控制疼痛,但治疗价格昂贵,也会发生植入电极移位、断裂、感染等并发症。
颈2神经节切除术是手术治疗方式的一种,但以前的手术方式是显微镜开放手术,需要较大的枕颈部手术切口,广泛的椎旁肌肉分离,才能获得足够的手术视野,暴露颈2神经节。这会导致术后切口肌肉疼痛、延缓恢复,从而影响手术效果。
余勇副主任医师团队创新地利用了经皮穿刺脊柱内镜的技术特点,只需在皮肤上开一个7mm的穿刺小切口,就可以把带有高清摄像头的手术通道送到颈2神经节附近,在高清晰度的手术视野的监视下,安全有效地切除颈2神经节,从而阻断枕神经的信号传递,解除病痛。
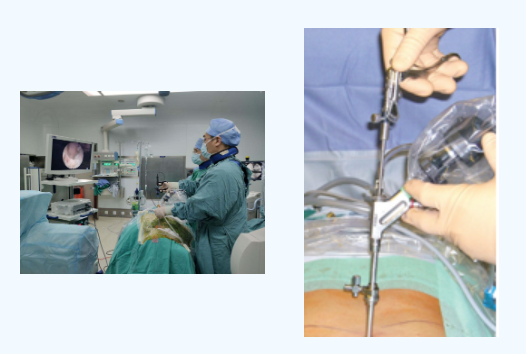
手术示意图、内镜示意图
近年来,中山医院神经外科脊柱脊髓亚专业发展迅速,尤其是脊柱内镜技术,在全国处于领先地位。作为中华医学会神经外科分会脊柱脊髓外科培训基地,科室举办了多期脊柱内镜全国培训班,培训了来自全国的脊柱内镜专科医生约200名。余勇副主任医师还参编重要脊柱内镜专著;担任外科前沿杂志(Frontiers in surgery)的客座主编,主编了脊柱内镜专刊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新突破#
65
👍
66
#微创#
64
#中山医院#
61
👍
62