CTO:首次观察到微环境CTCs的抗药治疗及转移
2012-01-22 MedSci MedSci原创
(从一位乳腺癌患者体内分离到的循环肿瘤细胞,CTCs) 2012年1月16日,据《每日科学》报道,德国肿瘤基因组研究中心(GENYO)的研究人员已经鉴定出能导致肿瘤发展和转移的基因变化及表型变化。肿瘤转移的过程--这是癌症致死的主要原因,是由肿瘤细胞入侵与最初受染器官无解剖学关系的远处器官所致。为了做到这一点,这些肿瘤细胞(称之为"循环肿瘤细胞",CTCs)有必要通过血液循环到达这些远处的器官。
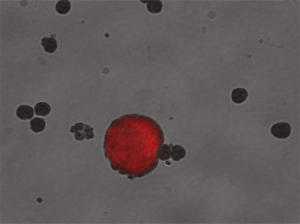
(从一位乳腺癌患者体内分离到的循环肿瘤细胞,CTCs)
2012年1月16日,据《每日科学》报道,德国肿瘤基因组研究中心(GENYO)的研究人员已经鉴定出能导致肿瘤发展和转移的基因变化及表型变化。肿瘤转移的过程--这是癌症致死的主要原因,是由肿瘤细胞入侵与最初受染器官无解剖学关系的远处器官所致。为了做到这一点,这些肿瘤细胞(称之为"循环肿瘤细胞",CTCs)有必要通过血液循环到达这些远处的器官。
研究人员在一位接受全身性治疗的乳腺癌患者体内检测到了正在进行细胞分裂的循环肿瘤细胞(CTCs)。从而证明循环肿瘤细胞(CTCs)能够适应诸如血液这样的恶劣环境,抵抗药物治疗并在其他组织和器官中分裂和增殖,最终导致转移。到目前为止,还没有在这类微环境中观察到这种行为。
研究的结果发表在Cancer Biology & Therapy、Clinical Translational Oncoloy及Annals of Oncology上,文章题目为"Biodynamics of Circulating Tumor Cell, Tumor Microenvironment and Metastasis(循环肿瘤细胞、肿瘤微环境及转移的生物动力学)"。研究人员发现循环肿瘤细胞(CTCs)处于基线水平的乳腺癌患者倾向于发生转移并在治疗后有较短的无病生存期(Disease-Free Survival,DFSs)。因此,在治疗期间及治疗后检测循环肿瘤细胞(CTCs)使医生能够识别哪些患者对化疗有积极的回应。结果,含有循环肿瘤细胞(CTCs)的患者尽管接受了化疗,只有一个较短的无病生存期和较低的总生存率(Overall Survival Rate,OSR)。这是由于这些循环肿瘤细胞(CTCs)对依据肿瘤的遗传学特征而开展的常规治疗有抵抗作用。因此,CTCs能够逃过化疗并转移到其他器官。
更有效的个性化治疗
格拉纳达大学教授、GENYO经理主任及研究组的协调员José Antonio Lorente博士确信,循环肿瘤细胞(CTCs)的研究至关重要,不仅因为它们负责转移的发生,还因为它们与原发肿瘤细胞和转移细胞有不同的遗传学特征。这种特征使这些极具侵略性的细胞能够抵抗机体的免疫系统及常规的化疗药物。"这些治疗大多针对的是肿瘤细胞的增殖。相反,循环肿瘤细胞(CTCs)被发现处于一种"冬眠"阶段,例如"非增殖"阶段。
由于这些细胞可能指示对治疗的阴性反应,如果将它们分离出来并进行遗传学鉴定,就可以根据复发的机会对患者进行分类,进行后续的个性化治疗。
"Biodynamics of Circulating Tumor Cell, Tumor Microenvironment and Metastasis"研究组由María José Serrano Fernández, José Luis García Puche, Pedro Sánchez Rovira, Juan Carlos Alvarez, Lucas González Herrera, Laura Vera Rodríguez, José Javier López Caballero and José Antonio Lorente组成。该研究小组已经对这项研究结果进行了相关的专利注册。该国际性项目依赖于罗氏制药、盘古(Pangaea)及Tromso大学(挪威)Inigo Martínez Zubiau教授的参与。(生物谷bioon.com)
Circulating tumour cells in peripheral blood: potential impact on breast cancer outcome.
Serrano MJ, Lorente JA, Delgado Rodríguez M, Fernández A, Fernández M, de la Torre C, Fernández Izquierdo J, Sánchez Rovira P.
Abstract: INTRODUCTION: In breast cancer, the metastatic process may involve the dissemination of circulating tumour cells (CTCs) through the blood and lymphatic system prior to the colonisation of distant organs. Here we demonstrate the predictive capacity of CTCs for detecting risk of death in breast cancer patients during established time intervals. METHODS: CTCs were identified by immunocytochemical methods following isolation by selective immunomagnetic cell separation of cytokeratin-positive cells. Serial blood samples from 65 patients were collected at roughly monthly intervals for up to 50 months. Follow-up was conducted at different intervals: 1-5, >5-12, >12-24 and >24-50 months. RESULTS: Both presence and number of CTCs were correlated to risk of death: patients with CTCs at any time during follow-up had a higher risk of death (p=0.035) than patients without CTCs. Furthermore, during the first 5 months of therapy, patients with >5 CTCs had a higher risk of death than patients with <5 CTCs (p=0.002). CONCLUSIONS: Our results show that the persistence of CTCs after chemotherapy, particularly during the first 5 months, could define a group of patients with a high risk of relaps.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CTC#
75
#CTO#
84
#TCS#
84
#CTCs#
73