BMJ:一例疑似咳嗽和上呼吸道感染患者
2016-04-16 MedSci MedSci原创
女性患者,82岁,因出现发痒咳嗽和上呼吸道感染症状而就诊。其血氧饱和度正常,也没有其他的系统性疾病。然而,患者有结核病病史,且多年前曾接受手术治疗,具体手术未知。经检查,医生发现患者右肺尖处呼吸声降低,建议胸部摄影检查。胸片显示如下(图1⇓)
女性患者,82岁,因出现咽喉发痒咳嗽和上呼吸道感染症状而就诊。其血氧饱和度正常,也没有其他食物系统性疾病。然而,患者有结核病病史,且多年前曾接受手术治疗,具体手术未知。经检查,医生发现患者右肺尖处呼吸声降低,建议胸部摄影检查。胸片显示如下(图1⇓)

诊断:患者右肺尖上部存在曾用来治疗肺结核的油胸。
讨论:没有任何迹象或其他病因显示患者的症状为上呼吸道感染所致。
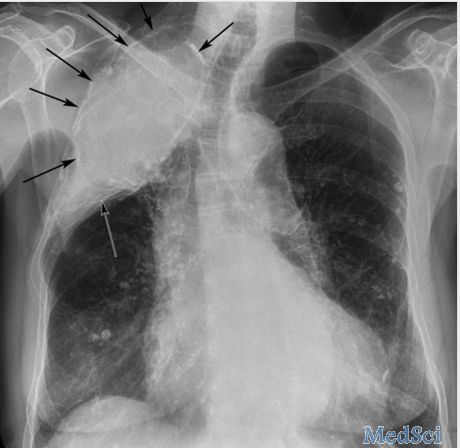
患者右侧肺尖处可见油胸(图2⇓,箭头),边界清楚,周边部分钙化。病灶为圆形,有囊壁围绕,位于胸膜外。挤压相邻的肋骨,导致肋骨拥挤,由于长期的体积损失使得肋骨变得纤细。右肺上叶体积丧失的其他可见特征包括右肺门上移和纵隔右移。
原始出处:
David C Howlett, Joseph Dalby Sinnott, Mild cough and decreased breath sounds in an 82 year old woman. BMJ 2016; 353 doi: http://dx.doi.org/10.1136/bmj.i2080 (Published 15 April 2016)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMJ#
76
#呼吸道#
111
学习了,谢谢!
123
文章不错
136
值得学习
125
学习了,值得
188