EUR J Cancer:FOLFOXIRI联合贝伐单抗治疗肝脏限制性转移性结直肠癌的疗效观察
2017-12-31 MedSci MedSci原创
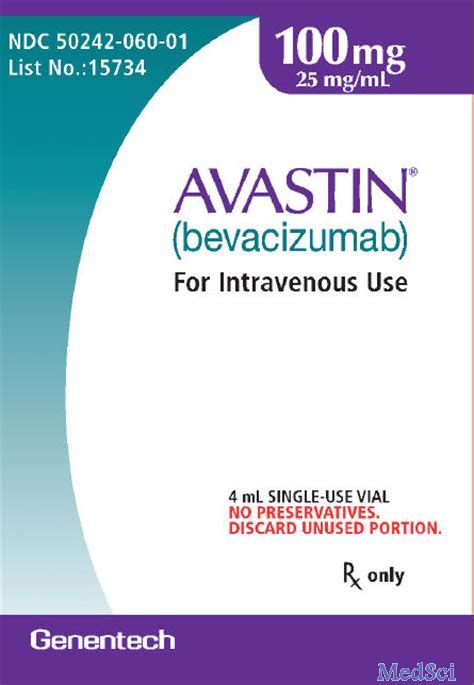
二次切除是治愈转移性结直肠癌(mCRC)中不能切除的肝脏限制性亚组患者的一个机会。肿瘤治疗的双重目标包括诱导肿瘤组织缩小和预防疾病的复发。FOLFOXIRI(亚叶酸,5-氟尿嘧啶,奥沙利铂和伊立替康)目前仍为一种标准化疗方案,在此研究人员分析评估了FOLFOXIRI联合贝伐单抗对肝脏限制性转移性结直肠癌的疗效,并调查了该治疗方案是否可以逆转高危患者的不良预后。
二次切除是治愈转移性结直肠癌(mCRC)中不能切除的肝脏限制性亚组患者的一个机会。肿瘤治疗的双重目标包括诱导肿瘤组织缩小和预防疾病的复发。FOLFOXIRI(亚叶酸,5-氟尿嘧啶,奥沙利铂和伊立替康)目前仍为一种标准化疗方案,在此研究人员分析评估了FOLFOXIRI联合贝伐单抗对肝脏限制性转移性结直肠癌的疗效,并调查了该治疗方案是否可以逆转高危患者的不良预后。
在541例患者中,有205例(37.9%)为肝脏限制性mCRC。74名患者(36.1%)接受了转移瘤的R0或R1切除。17名患者(8.3%)接受了R2切除。在单变量和多变量分析中,相比于其他患者,R0 / R1切除的患者具有显著延长的中位无进展生存期(PFS)(18.1 vs 10.7个月,HR:0.48 [0.35-0.66],p <0.001)和总生存期(OS)(44.3 vs 24.4个月,HR:0.32 [0.22-0.48],P <0.001)。R0切除的患者的5年PFS和OS率分别为12%和43%。
综上所述,综合长期试验结果和预后因素,FOLFOXIRI联合贝伐单抗治疗肝脏限制性转移性结直肠癌是安全有效的。
原始出处:
Cremolini,
Chiara, et al. "Efficacy of FOLFOXIRI plus bevacizumab in liver-limited
metastatic colorectal cancer: A pooled analysis of clinical studies by Gruppo
Oncologico del Nord Ovest." European Journal of Cancer 2017 73: 74-84.
doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#转移性#
41
#结直肠#
52
#FOLFOX#
0
#贝伐#
30