Nat Med:临床使用光遗传手段,部分恢复失明患者视觉
2021-05-25 haibei MedSci原创
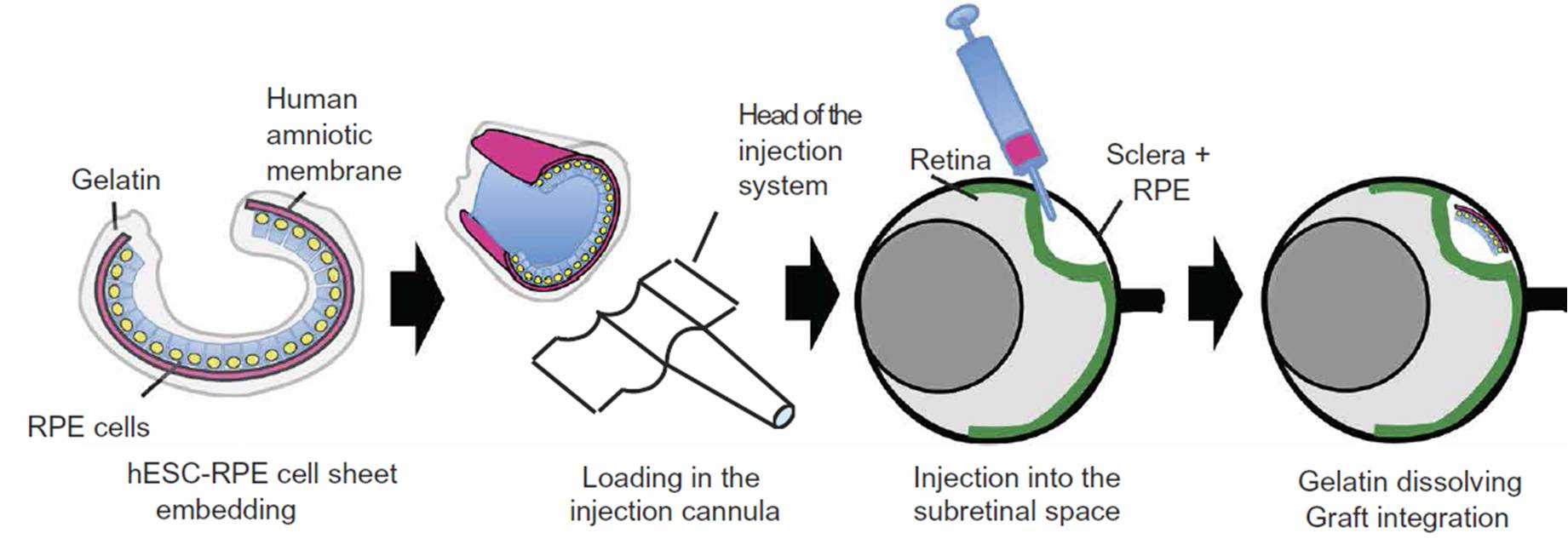
最近,在一个盲人患者身上,研究人员将眼内注射编码ChrimsonR的腺相关病毒载体与通过工程护目镜进行的光刺激相结合。护目镜检测局部的光强度变化,并将相应的光脉冲实时投射到视网膜上。
视网膜色素变性(RP)是一种进行性的、遗传性的、多数为单基因的致盲疾病,由超过71个不同基因的突变引起(https://sph.uth.edu/retnet/sum-dis.htm)。它影响着全世界200多万人。除了对一种由基因RPE65突变引起的早发RP的基因替代疗法外,目前还没有批准的RP疗法。
光遗传视力恢复是一种独立于基因突变背景的方法,可以用于恢复RP后期视力丧失后的视觉功能。开放标签的1/2a期PIONEER研究(ClinicalTrials.gov临床号:NCT03326336)旨在评估一种针对晚期非综合症RP患者的研究性治疗方法的安全性(主要目标)和有效性(次要目标),该方法结合了注射光遗传载体(GS030-药物产品(GS030-DP))和佩戴医疗设备,即光刺激护目镜(GS030-医疗设备(GS030-MD))。GS030-DP的概念证明和PIONEER临床试验中使用的GS030-DP剂量是在非人灵长类动物研究中确定的。

最近,在一个盲人患者身上,研究人员将眼内注射编码ChrimsonR的腺相关病毒载体与通过工程护目镜进行的光刺激相结合。护目镜检测局部的光强度变化,并将相应的光脉冲实时投射到视网膜上,以激活光遗传学转导的视网膜神经节细胞。
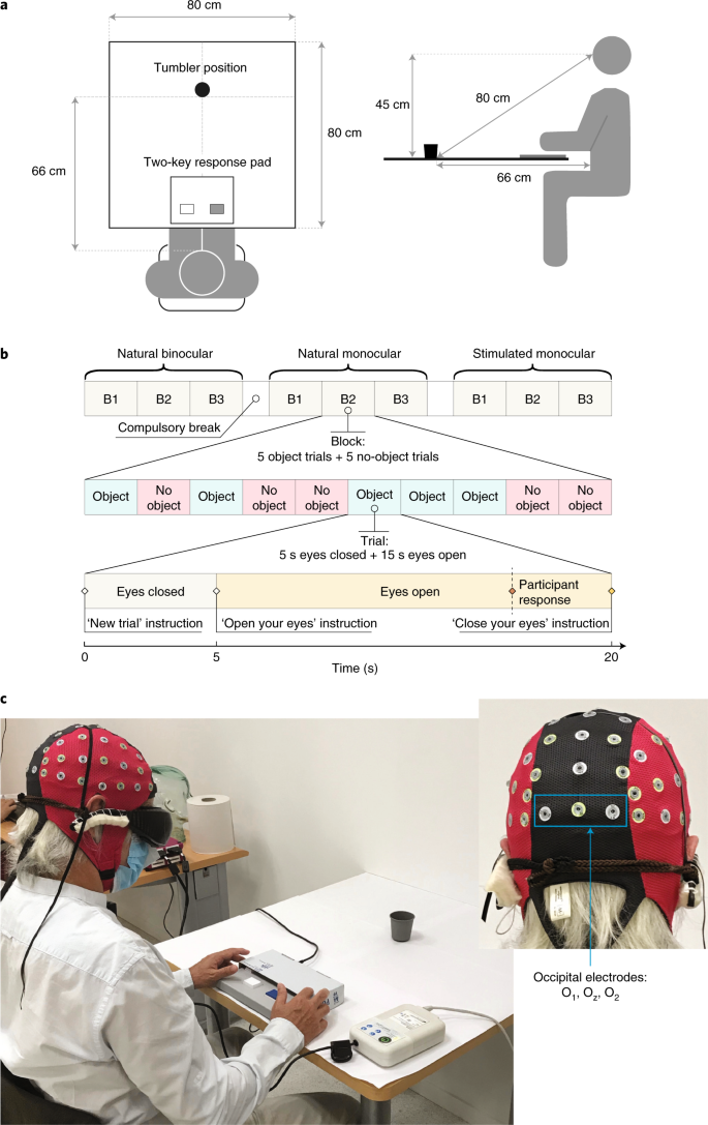
视觉任务与脑电图记录的综合测试
患者在佩戴护目镜时,仅用经过矢量处理的眼睛就能感知、定位、计数和触摸不同的物体。在视觉感知过程中,多通道脑电图记录显示了视觉皮层上方与物体有关的活动。
研究人员还证明,注射编码ChrimsonR的腺相关病毒载体与工程护目镜缺一不可,否则患者无法在视觉上发现任何物体。
总之,这是第一个报道的神经退行性疾病在光遗传治疗后部分恢复功能的案例。
原始出处:
José-Alain Sahel et al. Partial recovery of visual function in a blind patient after optogenetic therapy. Nature Medicine (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
57
厉害
70
#临床使用#
70
#光遗传#
82
#视觉#
77
#Med#
46
棒
82
医学发展带来希望
83
学到了!!
74