ASH2017前瞻:多发性骨髓瘤(MM)争议问题解答新进展
2017-12-02 HEADofHEMA HEADofHEMA
近年来随着临床研究的进展,多发性骨髓瘤新药不断涌现,包括免疫调节剂来那度胺、泊马度胺;蛋白酶体抑制剂硼替佐米、Carfilzomib、Ixazomib;单克隆抗体Daratumumab、Elotuzumab等。随着新药的涌现,多种治疗方案应用于临床,但一系列争议性的问题也摆在了临床医生的面前,在即将开幕的ASH 2017年会上,研究者们也将就相关问题进行了探讨。1. 对于高危MM患者
近年来随着临床研究的进展,多发性骨髓瘤新药不断涌现,包括免疫调节剂来那度胺、泊马度胺;蛋白酶体抑制剂硼替佐米、Carfilzomib、Ixazomib;单克隆抗体Daratumumab、Elotuzumab等。随着新药的涌现,多种治疗方案应用于临床,但一系列争议性的问题也摆在了临床医生的面前,在即将开幕的ASH 2017年会上,研究者们也将就相关问题进行了探讨。
1. 对于高危MM患者,来那度胺VS硼替佐米哪个更好?
Abstract 744对GIMEMA-MM-03-05研究和EMN01研究进行了亚组分析。GIMEMA-MM-03-05研究中患者随机分为两组,分别接受9个疗程硼替佐米-马法兰-泼尼松-沙利度胺后使用硼替佐米-沙利度胺维持治疗(VMPT-VT)或9个疗程VMP方案治疗;EMN01研究中患者随机分为三组,分别接受马法兰-泼尼松-来那度胺(MPR)或环磷酰胺-泼尼松-来那度胺(CPR)或来那度胺+低剂量地塞米松(Rd)治疗9个疗程,随后用来那度胺单药或联合泼尼松维持治疗。本摘要对这两项研究中的患者分别根据遗传学特征、年龄、性别、KPS评分和LDH水平进行亚组分析,比较硼替佐米和来那度胺的PFS和OS。在总共1163例患者中,902例患者有细胞遗传学数据,其中243例归入高危组,659例归入标危组。结果发现,在具有高危遗传学特征[del17p, t(4;14), t(14;16)]的患者中,采用硼替佐米治疗的中位PFS为30.8个月,来那度胺组为14.8个月(HR: 0.54; 95%CI: 0.41-0.72);在标危组中,中位PFS的差异较小,硼替佐米组为29.1个月,来那度胺组为22.1个月(HR: 0.87; 95%CI: 0.72-1.05)。在高危组中,硼替佐米降低了患者的总体死亡风险,中位OS为62.4个月而来那度胺组为43.2个月(HR: 0.68; 95%CI: 0.47-0.96);在标危组中,硼替佐米与来那度胺治疗未显示出OS的差异。
总体而言,这项对既往重要随机对照研究的亚组分析显示,对于高危MM患者,硼替佐米较来那度胺有PFS和OS的优势。

印度的一项随机对照III期研究(Abstract 906)比较了VRd(硼替佐米-来那度胺-地塞米松)和Ld(来那度胺-地塞米松)治疗新诊断MM的ORR、PFS和OS。根据ISS和LDH水平,本研究中大部分患者为III期患者,VRd组(n=74)中占81%,Ld组(n=69)占65%。结果发现VRd组的ORR(sCR+CR+VGPR+PR)为78.4%,略高于Ld组,但两组没有统计学差异。中位OS为30.2个月vs 28.6个月,中位PFS为27.8个月vs 28个月,均没有统计学差异。
这项研究未能证明其在Ld方案基础上加入硼替佐米有生存优势,其结果与2016年的SWOG S0777研究有所矛盾,该研究显示在Ld基础上加入硼替佐米可以显著延长患者的PFS(43个月 vs 30个月,HR 0.712, P=0.018)和OS(75个月 vs 64个月,HR 0.709, P=0.025)。本研究从数据上看VRd组的ORR和OS均略优于Ld组,之所以没有统计学差异可能是由于样本量较小的关系,每组仅有70例左右,远远少于SWOG S0777研究中每组260例以上的样本量。此外从患者的基线构成来看,本研究中VRd组III期患者明显多于Ld组,且本研究中III期患者的比例达65%以上,远高于SWOG S0777研究(33%),III期患者本身预后较差,生存期短(SWOG S0777研究中患者的生存期比本研究中患者长1倍还多),这也是导致PFS/OS没有差异的原因之一。本研究中VRd组能够在有更多预后较差的III期患者的情况下取得和Ld组相似的PFS和OS也在一定程度上说明在Ld方案基础上加用硼替佐米还是有可能获益的。
2. 适合移植的老年MM患者选择何种诱导方案?
Abstract 3161回顾性分析了86例65-75岁一线接受ASCT治疗患者的数据,患者采用硼替佐米为基础的方案(VTD 91%, VD 7%, VCD 2%)作为诱导方案,移植预处理采用马法兰 200mg/m2(MEL 200),马法兰剂量可根据年龄、合并症和身体状况减量至140或100mg/ m2。结果显示,在首次ASCT后,全体患者的CR率为34%, VGPR率为39%,73%的患者获得CR或VGPR。4级非血液学毒性发生率为16%,移植相关死亡率为0%。生存分析显示,患者2年PFS和OS分别为75%和91%。根据年龄的亚组分析显示,65-69岁组和70岁及以上组的PFS和OS无统计学差异。采用MEL200预处理的患者较减量预处理的患者有更好的生存,2年PFS分别为86%和57%(P=0.036),2年OS分别为100%和82%(P=0.005)。采用VTD诱导+MEL200预处理的51例患者OS未达到。
这项单中心研究提示,适合移植的老年MM患者可成功接受VTD诱导方案,并取得较好的生存结果,移植的最大年龄可达75岁。3. 不适合移植的老年MM患者如何治疗?
日本的一项多中心II期研究(Abstract 3162)纳入47例不适合移植的65岁以上MM患者,根据VES-13量表评估患者的身体状况,分为强健组(n=16)和虚弱组(n=31),强健组患者接受4个疗程标准剂量sVCD方案(皮下注射硼替佐米+环磷酰胺+地塞米松)随后4个疗程sVTD方案(皮下注射硼替佐米+沙利度胺+地塞米松),虚弱组患者采用相同方案和疗程数,但减低用药剂量。研究的主要终点为客观应答率(ORR)。结果显示,所有47例患者的ORR为87.2%,其中≥CR为17.0%,≥VGPR为46.8%;强健组患者的ORR为87.5%,其中≥CR为18.8%,≥VGPR为56.3%;虚弱组患者的ORR为87.1%,其中≥CR为16.2%,≥VGPR为41.9%。虚弱组3/4级不良事件多于强健组,但未发生没有预期到的不良事件。最常见的3/4级不良事件为贫血、中性粒细胞减少症、低钠血症和血小板减少症。
本项II期研究提示,个体化、剂量调整的三联序贯疗法在老年体弱患者中显示出高应答率和较好的安全性。这种以老年评估为指导的治疗方法在强健和体弱MM患者中均可能取得理想的结果。
4. 复发难治性MM患者有无改良的方案?
对于复发难治性MM,强化的细胞毒化疗VDT-PACE方案(硼替佐米、地塞米松、沙利度胺、顺铂、多柔比星、环磷酰胺和依托泊苷)及其改良方案(统称VPLRs方案)被一些研究作为整体治疗方案的一部分。
美国梅奥诊所的一项回顾性研究(Abstract 3096)分析了该诊所从2006年到2017年间143例采用VPLRs方案治疗的MM患者数据,其中141例为复发难治患者,2例为新诊断患者。在135例可评价的患者中,在1个疗程VPLRs方案治疗后,65.2%的患者至少获得最小应答(MR),至少获得PR的比例为51.1%,至少获得VGPR的比例为7.4%。在完成全部1-9个疗程VPLRs方案治疗后,至少获得MR、PR和VGPR的患者比例分别为68.9%、54.8%和10.4%。生存分析显示估计的中位PFS为3.1个月,中位OS为8.1个月。116例患者在VPLRs方案治疗后接受后线系统性化疗或SCT治疗,接受SCT患者的中位OS为15.1个月,显著好于接受化疗的患者的7.3个月(P<0.01)。分层分析显示年龄≥60岁和RISS III期与OS缩短相关。
梅奥诊所的研究证实VPLRs方案用于治疗复发难治性MM是有效的;VPLRs方案后采用SCT治疗可以获得更长的OS;年龄≥60岁和RISS III期预示OS缩短。
5. 生化复发患者应该再治疗还是等待观察?
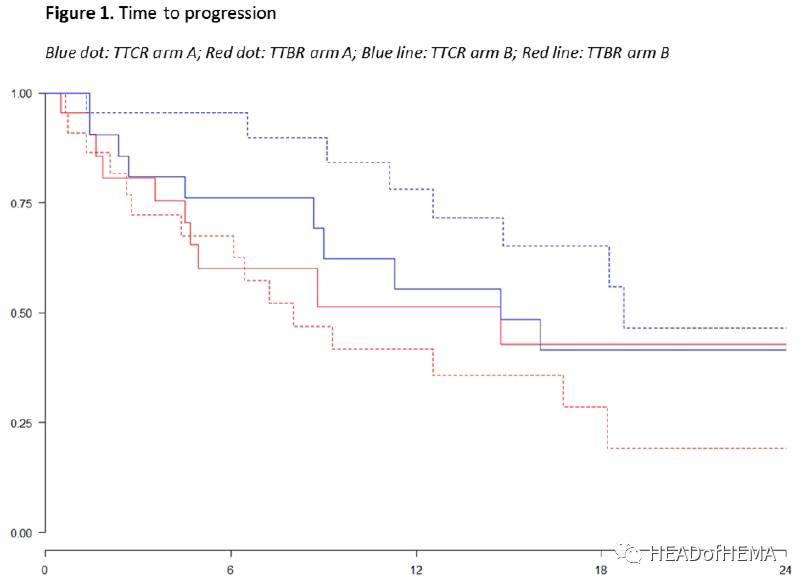
Abstract 3128比较了MM患者生化复发时早期采用Vd方案再治疗或等待观察的疾病进展时间(TTP),次要终点为PFS、OS和ORR。46例1-3线治疗复发或难治的患者被随机1:1分成两组,A组患者在生化复发时采用6个疗程Vd方案再治疗,B组患者在生化复发时采用等待观察。中位随访15.7个月后,A组和B组患者中分别有15例和11例发生生化复发,采用Vd方案再治疗且可评估的12例患者中2例(17%)获得VGPR,4例(33%)获得PR,2例(17%)疾病稳定(SD),另有4例(33%)疾病进展(PD)。而在等待观察的11例患者中,9例发生临床复发,只有2例仍维持无症状。在主要终点TTP方面,两组1年无生化复发率(TTBR)分别为42%和51%(HR 1.22,P=0.61),1年无临床复发率(TTCR)分别为78%和55%(HR 0.54,P=0.19)。
本研究提示,对于生化复发的MM患者,早期采用Vd方案再治疗是可行的,与等待观察相比可延缓疾病临床进展。
综合以上ASH 2017的新进展,我们可以看到一些争议性问题新的解决方案,包括硼替佐米为基础的方案在高危遗传学特征患者中的生存获益,VTD方案用于老年患者ASCT的诱导,个体化三联序贯疗法用于不适合移植的老年患者,VPLRs方案用于复发难治性MM的治疗,生化复发时采用Vd方案再治疗。我们也期待着ASH 2017的正式开幕,并带给我们更多的精彩内容!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
67
#ASH#
72
内容丰富.值得学习
103
学习了
105
血液肿瘤治疗中不规范的很多
113
谢谢分享.学习了谢谢分享.学习了
103
学习了新知识
124
好好好好好好好好
73
学习了
62
谢谢分享学习了
60