Circulation:早期使用NAC和NTG治疗可以减少STEMI患者PCI术后心肌梗死面积!
2017-06-21 xing.T MedSci原创
由此可见,大剂量静脉注射NAC同时接受低剂量静脉注射NTG与STEMI患者PCI术后心肌梗死面积减少相关。需要一个更大型的研究来评估这种疗法对临床心脏结局的影响。
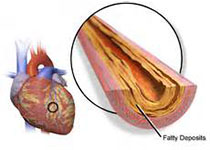
目前ST段抬高型心肌梗死(STEMI)的治疗包括经皮冠状动脉介入治疗(PCI),仍在继续的研究也专注于利用辅助疗法减少心肌梗死面积。N-乙酰半胱氨酸(NAC)是一个抗氧化剂,具有清除活性氧簇的特性,也可加强硝酸甘油(NTG)的作用,因此在PCI的辅助治疗中具有潜在的益处。NACIAM试验(NAC在急性心肌梗死中的作用)评估了NAC对接受PCI治疗的STEMI患者心肌梗死面积的影响。该研究是一项随机双盲、安慰剂对照、多中心临床研究,评估了在背景剂量NTG(2天,7.2mg)的基础上静脉注射大剂量NAC(2天,29g)对早期心脏磁共振(CMR)成像评估的心肌梗死面积的影响。该研究的次要终点包括CMR测定的心肌挽救水平,以及肌酸激酶(CK)动力学。该研究共有112名STEMI患者随机分组,75例患者(37例接受NAC治疗和38例接受安慰剂治疗)进行了早期CMR成像检查。缺血预处理的中位持续时间为2.4小时。所有患者给予了基础NTG输液,随机分配接受NAC治疗的受试者相比于安慰剂组受试者CMR评估梗死面积绝对减少了5.5%(中位数为11% vs. 16.5%;P=0.02)。在NAC组心肌挽救
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#PCI术#
81
#STEMI患者#
60
#STEM#
56
#PCI术后#
62
一起来学习吧
65