BMJ:原发性肺癌乳腺转移-案例报道
2017-04-10 xing.T MedSci原创
转移至乳房的肿瘤相对罕见,只占原发性肿瘤转移的0.5%- 2%。这个病例强调了考虑将非原发性乳腺癌作为一种鉴别诊断的重要性,因为其治疗与原发性乳腺癌有所不同。
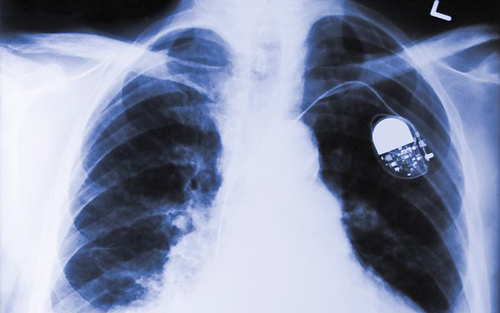
患者为一名63岁的女性,因其左乳房发现肿块而到乳房诊所就诊。通过临床体格检查、钼靶X线检查和核心活检证实肿块是腺癌,但它不是典型的原发性乳腺癌。
胸部计算机断层扫描以及随后的采用TTF-1免疫组化染色证实乳腺肿块(如图1中箭头1所示)为隐匿性原发肺癌转移(如图1中箭头2所示)。
转移至乳房的肿瘤相对罕见,只占原发性肿瘤转移的0.5%- 2%。这个病例强调了考虑将非原发性乳腺癌作为一种鉴别诊断的重要性,因为其治疗与原发性乳腺癌有所不同。
原始出处:
Zoe Barber, et al. Breast metastases from primary lung cancer.BMJ 2017; 357 doi: https://doi.org/10.1136/bmj.j1203
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#乳腺转移#
82
#BMJ#
109
#原发性肺癌#
94
#原发性#
83
学习了
116
学习了涨知识
1