JAMA Neurol:视而不见——孤立性上丘病变后的视觉疏忽个案报道1例
2021-11-05 Naomii 网络
一名40多岁的妇女出现了一个局限右侧SC的小脓肿,这罕见病例的研究为SC在引导视觉注意和眼睛朝向对侧大脑半球的作用提供了直接证据,即SC不仅是下行视觉注意通路中的一个节点,而且是视觉注意关键神经底物。
基于非人类灵长类动物和其他物种的电生理数据,视觉注意模型预测:在人类中,中脑上丘(SC)代表着一个大型额叶-皮质下注意网络的最后下游结构。这一观点部分得到了人类案例研究的支持,即发生了包含SC在内的广泛脑损伤后,视觉空间注意力不集中,这通常被称为视觉疏忽。近日,有研究人员展示了一例罕见的、仅局限于SC的小病变患者,证实了该模型的预测。
SC主要接受对侧视觉半球、纹状皮质、前额叶皮质、额叶眼场和顶叶皮质的视网膜输入。它处理视觉输入,并控制头部和眼睛运动的方向,以响应视觉刺激。动物实验表明,SC也与注意机制有关。例如,猴子或猫的SC失活会导致对侧视野中出现的目标出现类似忽视的迹象。然而,一项对PubMed数据库的审查显示,到目前为止还没有直接证据表明SC的孤立损害会在人类中产生对侧视觉忽视。
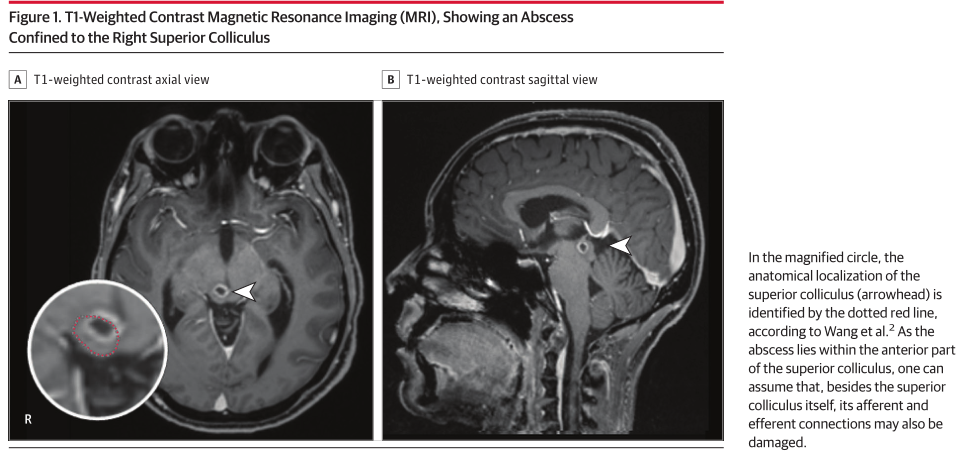
一名40多岁的妇女出现了一个局限在右侧SC的小脓肿(图1)。
SC的单边参与使研究人员能够观察到视觉注意分配的不对称性,直接证明了这一结构在视觉注意分配中的作用。实验方案采用了自由视觉探索范式,通过视觉注视的水平分布来量化左右半空间的视觉注意配置。研究人员预测,平均注视次数和累积注视持续时间将在左侧对侧减少,在右侧半球增加。此外,由于先前的数据显示忽视在早期注意方向上存在自我偏向,研究人员还检验了第一次扫视不会频繁地指向对侧左半球的假设。双侧dP值差异有统计学意义(P<0.05)。
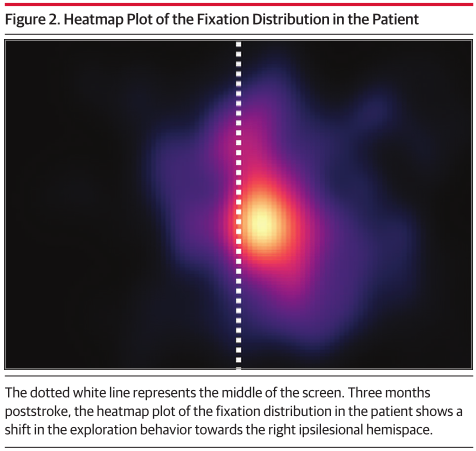
- 使用Singlims进行分析统计分析(图2),将患者的眼球运动数据与15名年龄和性别匹配的健康对照组(HC)的眼动数据进行比较,证实了假设,即左侧忽视,注视明显减少和较低的累积注视持续时间(患者:5.208;HC:平均[SD],10.858[1.422];t=Mean[SD],10.858[1.422];t=−3.848;P=0.002)。
- 右侧大脑半球内注视次数明显增多(患者:14.125;HC:平均注视[SD],11.223[1.265];t=2.222;P=0.04),累计注视持续时间显著增加(患者:4114毫秒;HC:平均注视[SD],2982[307]毫秒;t=3.573;P=0.003)。
- 患者第一次扫视明显较少指向对侧左半球(患者:8.333%;HC:平均[SD],61.677%[22.426%];t=−2.304;P=0.04)。
- 平均注视持续时间无差异(患者:左侧,290毫秒,右侧,291毫秒;HC:平均[SD],左侧,263[35]毫秒;t=0。7 65;P=0.46;右268[35]毫秒;t=0.641;P=.53)。
- 在诊断后9个月进行的随访测量显示,平均注视位置(0.978°)的忽略有所改善,但其他参数的病理结果的持续性(累计注视持续时间:左侧2151毫秒;t=−3.288;P=0.005;右侧3743毫秒;t=2.401;P=0.03;早期定位左侧8.333%;t=−2.304;P=0.04)。
对这一罕见病例的研究为SC在引导视觉注意和眼睛朝向对侧大脑半球方面的作用提供了直接证据,支持了这样的观点,即在人类中,SC不仅是下行视觉注意通路中的一个节点,而且实际上是视觉注意控制本身的关键神经底物。此外,这名患者在几个月后仍有忽视的证据,这一事实与猴子的皮层下视觉通路比人类更发达的观点是一致的。
文献来源:https://jamanetwork-com.fjny.80599.net/journals/jamaneurology/article-abstract/2785031
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#个案报道#
79
#Neurol#
68
#视觉#
83
#孤立性#
112