CCLM:miRNA在检验医学中的应用—血小板相关微小RNA的临床意义
2017-05-18 MedSci MedSci原创
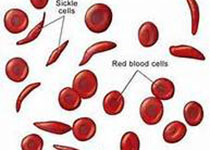
循环血小板在维持止血中起核心作用,参与越来越多的从动脉粥样硬化到癌症转移的病理生理过程。血小板衍生自骨髓巨核细胞,循环寿命为8-10天。它与许多粘附分子(包括与血小板表面受体相互作用的胶原)接触,导致血小板停滞和激活。一旦激活,血小板释放其颗粒物的含量以及二磷酸腺苷(ADP),血清素和血栓素A 2,导致进一步的血小板募集,聚集和栓塞形成。
近日,国际杂志Clinical Chemistry and
Laboratory Medicine上在线发表一期专辑介绍关于miRNA在检验医学中的应用的研究,阐述了miRNA在疾病病因学,诊断以及治疗中的作用和应用前景。本文介绍了血小板相关微小RNA的临床意义。
循环血小板在维持止血中起核心作用,参与越来越多的从动脉粥样硬化到癌症转移的病理生理过程。血小板衍生自骨髓巨核细胞,循环寿命为8-10天。它与许多粘附分子(包括与血小板表面受体相互作用的胶原)接触,导致血小板停滞和激活。一旦激活,血小板释放其颗粒物的含量以及二磷酸腺苷(ADP),血清素和血栓素A 2,导致进一步的血小板募集,聚集和栓塞形成。
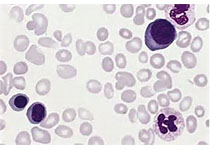
越来越多的证据表明血小板微小RNA对血小板生物发生很重要,囊泡相关膜蛋白8(VAMP8)/ endobrevin mRNA的水平升高与血小板过度反应相关,miR-96可调节培养细胞中的VAMP8 / endobrevin mRNA水平。这些数据进一步支持VAMP8 / endobrevin在血小板反应性异质性中的作用,并表明miR-96在调节VAMP8(参与血小板分泌过程的初级血小板v-SNARE蛋白)的表达中起作用。
与从细胞内释放的外泌体(<0.1μm)不同,血小板MP基本上是从细胞质膜脱落并表达抗原(例如CD41和CD62p)的血小板细胞质泡状结构(P选择素); 类似于外泌体和凋亡小体,它们可以基于大小与凋亡小体(>1μm)区分开。MPs能够表达磷脂酰丝氨酸,因此在释放期间发生膜不对称性丧失。所有这些标记物可以通过流式细胞术检测,并用于区分血小板MP与其它来自内皮细胞和红细胞的循环MPs。
血小板MP相关微小RNA在生物学和病理生理学各个方面的作用及其重要性越来越被认可。微RNA存在于人体的所有生物流体中,如唾液,尿液,鼻分泌物,精子和血浆,相对容易从患者收集。因此监测从患者收集的生物样品中的血小板特异性MP和微小RNA有助于确定微小RNA与特定疾病或病症之间的相关性,并进一步鉴定更敏感的生物标志物。
原始出处:
Patrick Provost, et.al. The clinical significance of platelet
microparticle-associated microRNAs.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#检验医学#
90
#miR#
67
#miRNA#
121
#微小RNA#
110
#小RNA#
96
学习了,谢谢分享
125
谢谢分享,学习了
119
感谢分享,学习了,
112
血小板的功能远远超出我们现在的想象,他与大部分肿瘤的转移都可能有关系
96