Clin Nutrition: 迷你营养评估简表是患有心力衰竭的门诊患者的病死率较好的预测工具
2020-11-15 MedSci原创 MedSci原创
营养状况是心力衰竭(HF)患者的重要预后因素。在一项研究中,研究人员观察到,与其他筛查工具相比,迷你营养评估简易表工具(MNA-SF)是筛查HF门诊患者营养状况的最佳方法。
背景与目标
营养状况是心力衰竭(HF)患者的重要预后因素。在一项研究中,研究人员观察到,与其他筛查工具相比,迷你营养评估简易表工具(MNA-SF)是筛查HF门诊患者营养状况的最佳方法。本项研究旨在确定MNA-SF是否对心衰患者具有预后价值,营养不良的影响是否因左心室射血分数(LVEF)而异。

方法
本项前瞻性研究是在一家大学医院的HF门诊就诊的患者中进行的。所有受试者在研究进入时均完成了MNA-SF测评。主要观察终点是全因死亡率。次要终点是复发性HF相关住院的次数以及全因死亡或HF相关住院的综合终点。营养不良和有营养不良风险的患者合并在一起,并对其营养状况异常以进行统计分析。
结果
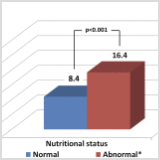
从2016年10月到2017年11月,共纳入555名患者(年龄69±11.5岁,男性71%,LVEF 44.6±13.2)。在103名(18.6%)受试者中发现了异常的营养状况。在平均23.8±6.6个月的随访期间,有99例患者死亡(17.8%),74例因心力衰竭住院(13.3%),复合终点为181例(32.6%)。在单变量分析中,营养不良与总人群的全因死亡率(p = 0.02)和复合终点(p = 0.02)显着相关。但是,在多变量分析中,包括年龄,性别,NYHA功能分类,BMI,缺血性病因,糖尿病,高血压和心衰持续时间,异常营养状况与全因死亡率(HR 3.32 [95%CI 1.47–7.52],p = 0.004)和复合终点(HR 2.53 [95%CI 1.30–4.94] ,p = 0.006)相关。营养状况异常的患者复发性心衰相关住院的总次数是原来的两倍(每100名患者年分别为16.4和8.4,p <0.001)。
结论
通过将MNA-SF用作常规筛查工具,可以在五分之一HF患者中检测到异常的营养状况。由MNA-SF评估的营养状况是门诊患者全因死亡和全因死亡或HF相关住院综合终点的独立预测指标。
原始出处:
Clara Joaquín. Et al. Mini Nutritional Assessment Short Form is a morbi-mortality predictor in outpatients with heart failure and mid-range left ventricular ejection fraction. Clinical Nutrition.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#病死率#
99
#门诊患者#
95
#nutrition#
89
简单快捷有意义
151
非常好的文章
132
学习了
131