JNNP: 不明原因栓塞性卒中患者的心房心脏病和非狭窄性颅内复杂动脉粥样硬化斑块
2021-12-09 MedSci原创 MedSci原创
未确定来源的栓塞性卒中(ESUS)一词用于描述在无明显近端动脉狭窄、主要心源性栓塞或其他特定病因的情况下发生的非腔隙性梗死。 隐匿性心房颤动最初被认为是ESUS的主要机制;然而,越来越多的证据表明,这
未确定来源的栓塞性卒中(ESUS)一词用于描述在无明显近端动脉狭窄、主要心源性栓塞或其他特定病因的情况下发生的非腔隙性梗死。 隐匿性心房颤动最初被认为是ESUS的主要机制。目前的证据表明,心房心脏病(AC)独立于心房颤动,在ESUS中是一个重要的潜在栓塞源。AC相关心电图(如V1导联P波终末力(PTFV1)、室上性早搏)、生化(如C反应蛋白、N端前体钠尿肽(NT-proBNP)和高敏心肌肌钙蛋白T(Hs-cTnT))和结构异常(如左房直径(LAD))与隐源性卒中/ESUS独立相关。主动脉、颅外和颅内非狭窄性动脉粥样硬化斑块,统称为心上动脉粥样硬化,作为ESUS中另一个显著的潜在栓塞源出现。最近研究报告,非狭窄性颅内复杂动脉粥样硬化斑块(NICAP)在梗死的同侧比对侧更普遍,支持NICAP在ESUS中的病因作用。
如果AC和同侧NICAP确实与ESUS有因果关系,则可以假设ESUS人群中存在这两种实体之间的负相关,但在其他中风人群中不存在这种负相关,这些人群在病因上与该实体无关,如因小血管疾病(SVD)导致的中风患者。本文旨在评估(1)在ESUS患者和SVD患者中AC和NICAP之间的相关性,以及(2)先前提出的生物标记物在确定AC为ESUS潜在病因方面的表现。本文发表在《神经病学,神经外科学和精神病学杂志》上()。
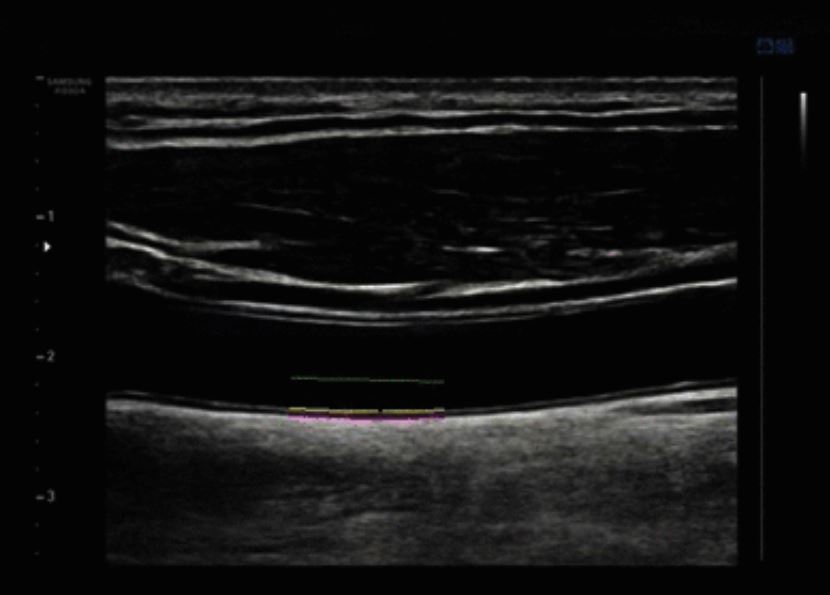
403名受试者(243名ESU和160名SVD)被纳入最终分析。所有患者均接受颅内HR-MRI以评估同侧NICAP的存在。入院后24小时内收集AC的生物标志物(即心电图上V1导联的P波终末力(PTFV1)、N-终末普罗布林钠尿肽(NT-proBNP)、高敏心肌肌钙蛋白T和左心房直径)。
SVD和ESUS患者PTFV1增加和HR-MRI结果
结果显示AC在ESUS患者和SVD患者中更为普遍,进一步支持了AC和ESUS之间的关系。此外,在ESUS患者中,与同侧NICAP患者相比,无同侧NICAP患者的AC更为普遍,这一发现在SVD患者中并不明显,进一步支持了ESUS中AC与动脉粥样硬化斑块的明显关系。此外,排除同侧NICAP患者后,AC/AC相关生物标记物在区分ESU和SVD方面的表现显著改善。此外,排除具有AC/AC相关生物标记物的患者后,同侧NICAP区分ESU和SVD的能力明显增强。总的来说,这些结果支持这样的观点,即AC是ESUS患者的一个重要病因,而非同侧NICAP。此外,,AC唯一信息量最大的生物标志物是PTFV1。
总之,与患有同侧NICAP的患者相比,患有ESUS但未患同侧NICAP的患者AC更为普遍,这意味着AC和同侧NICAP是ESUS的两种不同的的病因。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#粥样硬化#
91
#卒中患者#
67
#心房心脏病#
63
写的真好
178
希望早日找到来源
96
#斑块#
63
#动脉粥样硬化斑块#
55
#栓塞性卒中#
63
#心房#
61